What Are The Three Types Of Aki
There are many causes of AKI, including infections, heart disease, liver disease, autoimmune diseases, cancer, hypertension, and traumatisms. In short, causes are uncountable.
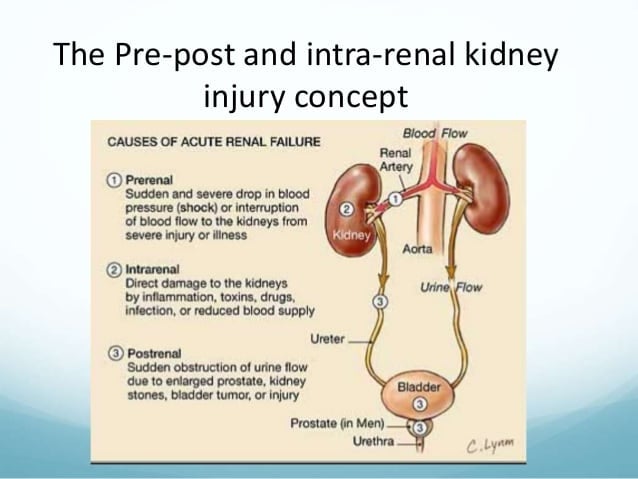
Having this many causes for a single condition can be overwhelming, even for experienced physicians. That is why the medical community divides AKI causes into three main categories prerenal AKI, intrinsic AKI, and post-renal AKI.
Every time a doctor faces an acute kidney injury, the first thing he will do is classified as prerenal, intrinsic, or extrinsic. Some AKI patients have mixed conditions with both an intrinsic and post-renal component.
Many times untreated AKI evolves to intrinsic AKI. Patients with chronic kidney disease can present a sudden worsening in their condition. This situation also classifies as AKI. Acute kidney injury often speeds up CKD.
How Do You Detox Your Kidneys
In the last few decades, kidney detoxing and kidney cleansing programs have gained a lot of popularity. However, so far, there isnt any convincing scientific evidence that cleansing programs do anything.
If there where toxins that are accumulating in your kidneys, that would mean you have uremia, and the only effective detox therapy, in that case, is dialysis.
Just remember drinking water every day and having a healthy diet. That is all the help your kidneys require from you.
Original Articlemild Elevation Of Urinary Biomarkers In Prerenal Acute Kidney Injury
Prerenal acute kidney injury is thought to be a reversible loss of renal function without structural damage. Although prerenal and intrinsic AKI frequently coexist in clinical situations, serum creatinine and urine output provide no information to support their differentiation. Recently developed biomarkers reflect tubular epithelial injury therefore, we evaluated urinary biomarker levels in an adult mixed intensive care unit cohort of patients who had been clinically evaluated as having prerenal AKI. Urinary L-type fatty acidbinding protein , neutrophil gelatinaseassociated lipocalin , interleukin-18 , N-acetyl–D-glucosaminidase , and albumin in patients with prerenal AKI showed modest but significantly higher concentrations than in patients with non-AKI. We also conducted a proof-of-concept experiment to measure urinary biomarker excretion in prerenal AKI caused by volume depletion. Compared with cisplatinum and ischemiareperfusion models in mice, volume depletion in mice caused a modest secretion of L-FABP and NGAL into urine with more sensitive response of L-FABP than that of NGAL. Although no histological evidence of structural damage was identified by light microscopy, partial kidney hypoxia was found by pimonidazole incorporation in the volume depletion model. Thus, our study suggests that new AKI biomarkers can detect mild renal tubular damage in prerenal acute kidney injury.
- Previous article in issue
Also Check: Can You Have 4 Kidneys
Acute Kidney Failure Prerenal Causes
Prerenal failure is the most common type of acute renal failure . The kidneys do not receive enough blood to filter. Prerenal failure can be caused by the following conditions:
- Dehydration: From vomiting, diarrhea, water pills, or blood loss
- Disruption of blood flow to the kidneys from a variety of causes:
- Drastic drop in blood pressure after surgery with blood loss, severe injury or burns, or infection in the bloodstream causing blood vessels to inappropriately relax
- Blockage or narrowing of a blood vessel carrying blood to the kidneys
- Heart failure or heart attacks causing low blood flow
- Liver failure causing changes in hormones that affect blood flow and pressure to the kidney
There is no actual damage to the kidneys early in the process with prerenal failure. With appropriate treatment, the dysfunction usually can be reversed. Prolonged decrease in the blood flow to the kidneys, for whatever reason, can however cause permanent damage to the kidney tissues.
Acute Kidney Injury And Extra

Recent evidence in both basic science and clinical research are beginning to change our view for AKI from a single organ failure syndrome, to a syndrome where the kidney plays an active role in the evolution of multi-organ dysfunction. Recent clinical evidence suggests that AKI is not only an indicator for severity of illness, but also leads to earlier onset of multi-organ dysfunction with significant effects on mortality. Animal models of renal injury have been used extensively in order to elucidate the mechanism of remote organ dysfunction after AKI despite their limitations due to interspecies differences. These studies have shown a direct effect of AKI on distant organs. These animal studies include models of ischaemiareperfusion injury and sepsis, mainly lipopolysaccharide endotoxin induced sepsis due to its reproducibility in creating distant organ failure. AKI is not an isolated event and it results in remote organ dysfunction to the lungs, heart, liver, intestines and brain through a pro-inflammatory mechanism that involves neutrophil cell migration, cytokine expression and increased oxidative stress . Three recent excellent reviews explore the mechanisms and the long-term consequences of AKI other organ systems.
Kidney-lung crosstalk in the critically ill patient
Heart-kidney crosstalk: the cardiorenal syndrome
Recommended Reading: What Laxative Is Safe For Kidneys
How Can I Prevent Acute Kidney Injury
Because AKI happens suddenly, it can be hard to predict or prevent it. But taking good care of your kidneys can help prevent AKI, chronic kidney disease and kidney failure/ESRD. Follow these general rules to keep your kidneys as healthy as possible:
- Work with your doctor to manage diabetes and high blood pressure.
- Live healthy! Eat a diet low in salt and fat, exercise for 30 minutes at least five days per week, limit alcohol and take all prescription medicines as your doctor tells you to.
- If you take over-the-counter pain medicines, such as aspirin or ibuprofen, do not take more than is recommended on the package. Taking too much of these medicines can hurt your kidneys and can cause AKI.
Diagnostic Tests & Interpretation
- Compare to baseline renal function .
- Urinalysis: dipstick for blood and protein microscopy for cells, casts, and crystals
- Sterile pyuria suggests AIN triad of fever, rash, and eosinophilia present in 10% of cases
- Proteinuria, hematuria, and edema, often with nephritic urine sediment , suggest GN or vasculitis.
- Casts: transparent hyaline castsprerenal etiology pigmented granular/muddy brown castsATN WBC castsAIN RBC castsGN
- Urine eosinophils: 1% eosinophils suggest AIN .
- Urine electrolytes in an oliguric state
- FENa = × 100
- FENa < 1%, likely prerenal > 2%, likely intrarenal
- If patient on diuretics, use FEurea instead of FENa: FEurea = × 100 FEurea< 35% suggests prerenal etiology.
Follow-Up Tests & Special Considerations
Read Also: Is Honey Good For Kidney Health
What Is The Treatment For Acute Kidney Injury
The treatment for AKI depends on what caused it to happen. Most people need to stay in the hospital during treatment and until their kidneys recover. While you are being treated for the problem that caused your AKI, you may also have treatments to prevent problems that can make it harder for your kidneys to heal. Some possible treatments include:
- Temporary hemodialysis to do the work that your kidneys should be doing, until they can recover
- Medicines to control the amounts of vitamins and minerals in your blood
- Treatments to keep the right amount of fluid in your blood
When you return home, your doctor may ask you to follow a kidney-friendly diet plan to help your kidneys continue to heal. Your doctor may be able to refer you to a dietitian, who can help you make a kidney-friendly diet plan that works for you.
Prerenal Acute Kidney Injury Must Know Drugs
Date March 20, 2019Author By Eric ChristiansonCategory Kidney
Prerenal acute kidney injury is absolutely something that happens in real life practice. One of the reasons that this is something that is seen on a somewhat regular basis is that the drugs that can cause prerenal acute kidney injury are very common.
Diuretics, Diuretics, Diuretics
Any medication that can promote the loss of fluid can cause dehydration, and ultimately prerenal acute kidney injury . Loop and thiazide diuretics are two extremely common medications that increase fluid loss out of the body and can cause dehydration. When the vessels dont have enough fluid in them, the blood pressure within the kidney falls. With inadequate pressure, the supply of nutrients and oxygen dwindles, leaving the kidney damaged and not functioning properly.
What makes things really challenging is when patients need diuretics for heart failure. There is a very delicate balance between running fluid off and running too much off and causing prerenal acute kidney injury.
ACE Inhibitors and ARBs
The exact mechanism of reducing that pressure in the glomerulus is through blocking vasoconstriction of the efferent arteriole. The efferent arteriole is the one that exits the glomerulus. If the pressure gets too low, this can lead to AKI.
NSAIDs
You can begin to understand how using all three of these agents together can really put a strain on the kidney and increase the risk of prerenal AKI.
Don’t Miss: Seltzer Water Kidney Stones
Acute Renal Failure In Children
Dilys A. Whyte, Richard N. Fine Acute Renal Failure in Children. Pediatr Rev September 2008 29 : 299307.
After completing this article, readers should be able to:
Define acute renal failure .
Differentiate the three forms of ARF.
Initiate treatment, including stabilization, of a patient who has ARF.
Discuss the various medications necessary for treating a patient who has ARF.
Acute renal failure is defined as an acute decline in renal function characterized by an increase in blood urea nitrogen and serum creatinine values, often accompanied by hyperkalemia, metabolic acidosis, and hypertension. Significant morbidity and mortality can accompany ARF. Patients who have ARF recover their renal function either partially or completely or they develop end-stage renal disease. They also may develop associated multiorgan disease.
ARF is divided into three forms: prerenal failure , intrinsic renal failure, and postrenal failure. Treatment ranges from conservative medical management to dialysis or renal transplantation, depending on the severity of…
B Common Pitfalls And Side
There are a few common pitfalls in the evaluation and management of pre-renal failure. Since the patients volume status is not always clinically clear in ineffective circulating volume states, there may be times where the decision between diuresis and volume resuscitation is difficult. If a patient has received more than a liter of isotonic intravenous fluids and the creatinine has not decreased, you can probably conclude that this is not isolated pre-renal failure due to a low circulating volume, although this has not been well studied. Reliance on the FENa should also not supersede good clinical judgement given its poor specificity and many potential confounders.
Recommended Reading: What Causes Kidney Problems In Humans
What Is The Kidney And What Does It Do
The kidneys are two coffee bean-shaped organs found in the posterior part of the abdominal cavity which name is retroperitoneum. They connect with the bladder through two thin muscle tubes called the ureters.
The kidneys primary function is to filter blood, remove excess fluid, electrolytes, and waste material to make urine. Urine flows from the kidneys to the bladder. Then, it goes from the bladder to the urethra and finally, from the urethra to the toilet.
The kidneys are vital in maintaining a healthy balance of electrolytes, fluids, acids, and bases in the body. They are also crucial in arterial tension regulation and are the target of important antihypertensive medications . Kidneys also produce essential hormones that control red blood cell production.
Each kidney is made up of millions of nephrons. Each nephron has two main parts the glomerulus and the tubule. The glomerulus is the filter, it works more or less in the same way as a coffee filter does. The tubule removes and adds different elements to the original filtrate according to the bodys needs.
For example, in the dehydrated person, the tubule will absorb a lot of the fluid from the original glomerular filtrate. If a person has excess acid in the body, the tubules will excrete that acid and reabsorb bicarbonate in turn. The substances and fluid the tubules do not reabsorb become urine that flows into the bladder.
Continue Learning About Kidney Failure
Important: This content reflects information from various individuals and organizations and may offer alternative or opposing points of view. It should not be used for medical advice, diagnosis or treatment. As always, you should consult with your healthcare provider about your specific health needs.
Also Check: How Much Money Is A Kidney Worth
Acute Kidney Failure Medications
The patient may be given medicines to treat the cause of the acute renal failure or to prevent complications.
- Antibiotics: To prevent or treat infections
- Diuretics : Quickly increase urine output
Acute Kidney Injury & Failure Symptoms Causes & Treatments
When your kidneys stop working suddenly, over a very short period of time , it is called acute kidney injury . AKI is sometimes called acute kidney failure or acute renal failure. It is very serious and requires immediate treatment.
Unlike kidney failure that results from kidney damage that gets worse slowly, AKI is often reversible if it is found and treated quickly. If you were healthy before your kidneys suddenly failed and you were treated for AKI right away, your kidneys may work normally or almost normally after your AKI is treated. Some people have lasting kidney damage after AKI. This is called chronic kidney disease, and it could lead to kidney failure if steps are not taken to prevent the kidney damage from getting worse.
Don’t Miss: Fluid Buildup Around Kidney
Preventing Acute Kidney Injury
Those at risk of AKI should be monitored with regular blood tests if they become unwell or start new medication.
It’s also useful to check how much urine you’re passing.
Any warning signs of AKI, such as vomiting or producing little urine, require immediate investigation for AKI and treatment.
People who are dehydrated or at risk of dehydration may need to be given fluids through a drip.
Any medicine that seems to be making the problem worse or directly damaging the kidneys needs to be stopped, at least temporarily.
The National Institute for Health and Care Excellence has produced detailed guidelines on preventing, detecting and managing AKI.
Who’s At Risk Of Acute Kidney Injury
You’re more likely to get AKI if:
- you’re aged 65 or over
- you already have a kidney problem, such as chronic kidney disease
- you have a long-term disease, such as heart failure, liver disease or diabetes
- you’re dehydrated or unable to maintain your fluid intake independently
- you have a blockage in your urinary tract
- you have a severe infection or
- you’re taking certain medicines, including non-steroidal anti-inflammatory drugs or blood pressure drugs, such as ACE inhibitors or diuretics diuretics are usually beneficial to the kidneys, but may become less helpful when a person is dehydrated or suffering from a severe illness
- you’re given aminoglycosides a type of antibiotic again, this is only an issue if the person is dehydrated or ill, and these are usually only given in a hospital setting
You May Like: Which System Do Kidneys Belong To
C Criteria For Diagnosing Each Diagnosis In The Method Above
The RIFLE criteria should be applied to a patient with suspected of acute renal failure to determine the degree of acute kidney injury and whether or not the patient is oliguric or not. The next step should be take a good history and determine if the patient is at risk for potential causes of pre-renal failure and if their physical exam supports one of these potential diagnosis. If the history and physical are suggestive of one of the low circulating volume states, empiric treatment with volume repletion can be initiated without further diagnostic tests.
What Tests To Perform
Serum creatinine concentration is the main test used to diagnose AKI. In non-steady state conditions such as AKI, the SCr concentration may not provide an accurate estimate of glomerular filtration rate because changes in SCr may lag by many hours. In the setting of AKI, daily measurements of SCr should be performed. More frequent measurements may be indicated in critically ill individuals.
The pattern of rise in SCr may be helpful diagnostically. Pre-renal azotemia usually leads to modest rises in SCr that return to baseline with treatment of the underlying condition. Contrast nephropathy typically leads to a rise in SCr within 24 to 48 hours, a peak within 3 to 5 days, and subsequent resolution within 5 to 7 days. Atheroembolic disease usually shows more subacute rises in SCr, though rapid increases may be observed in severe cases. Increases in SCr of 0.5 mg/dL or greater within 24 hours may reflect substantially reduced kidney function, and such patients should be monitored carefully.
Blood urea nitrogen increases in AKI but can also increase due to hypercatabolic states, upper gastrointestinal bleeding, hyperalimentation, and corticosteroid therapy. A disproportionate rise in BUN compared to SCr, in the absence of other causes of BUN elevation, may be observed in pre-renal azotemia.
Don’t Miss: Does Red Wine Cause Kidney Stones
What Pee Color Is Bad
In acute kidney injury, urine tends to turn very strong and dark. It can look very yellow, brown, or reddish. However, this does not occur in all cases of acute kidney injury.
Kidney failure is not the only cause of dark urine. Other diseases like pyelonephritis, hepatitis, biliary disease, and simple dehydration without AKI can also produce dark urine.
Hematuria can also present as brown urine. It should not be mistaken for dark urine due to any of the causes, as mentioned earlier.