Rh B And C Glycoproteins
Recently, new ammonia carriers have been identified in the kidney of mammals, i.e. the Rh B and C glycoproteins . RhBG and RhCG are nonerythroid homologs of the blood group Rh proteins which share significant sequence homology with the methyl-ammonium permease/ammonium transporters superfamily of primitive organisms. In the rat kidney, RhBG and RhCG are expressed in the basolateral and apical membranes, respectively, in the same cells of the distal nephron, i.e. all cells of the connecting tubule and intercalated cells of the cortical and medullary collecting ducts . When expressed in Xenopus laevis oocytes, RhCG was clearly shown to be a NH3 carrier but, because NH4Cl exposure induced inward currents in RhCG-expressing but not in control oocytes, it was suggested that RhCG also mediates electrogenic NH4+ transport . It must be emphasized, however, that AmtB of Escherichia coli has been recently demonstrated to form a trimer of channel-containing proteins which specifically conduct uncharged NH3, not NH4+. Thus, it is possible that, in the study cited above , exposure to NH4Cl of RhCG-expressing oocytes simply activated an endogenous NH4+ conductance after entry of NH3 within the oocytes . Whether RhBG and RhCG are involved in transepithelial ammonia transport and/or in ammonia accumulation within the cells to regulate the activity of other acid-base transporters in the distal nephron is not established at present.
Location Of Tubular Secretion
In humans, and other vertebrates, tubular secretion occurs in the kidneys, where the blood is filtered in specialized structures known as nephrons. These structures consist of a long tubule surrounded by extensive capillaries. The secreted substances come from the blood in peritubular capillaries and pass through the interstitial fluid before going through the wall of the tubule into the inside of the tubule . Different aspects of secretion occur in the proximal or distal portions of each tubule, but not in the region between known as the loop of Henle.
In the image above, a simplified drawing of a nephron within the kidney is shown. Secretion is indicated by the letter S, which involves specific waste products moving from the blood in the capillaries into the nephron tubule .
Uremic Toxins And Renal Tubular Transporters
Several organic anionic uremic toxins , which bind to serum albumin, are excreted from the kidneys by tubular secretion, and OATs play a central role in this process.26,27 However, hippuric acid, IS, and kynurenic acid inhibited MRP4 or BCRP uptake, while phenylacetic acid and indoleacetic acid only reduce MRP4 uptake. Conversely, quinolinic acid, oxalate, and putrescine did not alter transport mediated by MRP4 or BCRP.7 Besides, OCT2-mediated uptake is the first step in the kidney secretion of many cationic endogenous metabolites or xenobiotics, and its transport failure leads to cationic metabolites accumulation, phenomenon which has been associated with cardiovascular implications. In addition, it has been documented that OCT2-mediated uptake was inhibited by polyamine and guanidino cationic uremic toxins.4 Wikoff et al found that several substances, as is the case of IS, which derive from hepatic Phase II metabolism of enteric gut precursors and interact with the renal Oat1 transporter , accumulate in chronic nephropathy. This finding supports the existence of a complex and remote communication between the gut microbiome, liver metabolism, and elimination via renal Oats, as well as the importance of Oat1 in the endogenous toxins handling in uremia.28 Takada et al demonstrated that ATP-binding cassette transporter subfamily G member 2 is a major transporter of the uremic toxin IS and identify ABCG2 as an important factor influencing CKD progression.29
Don’t Miss: Is Ibuprofen Metabolized In The Kidneys Or Liver
What Is The Urinary System
The urinary system contains the kidneys, bladder, ureters, and urethra. These organs work together primarily to create, store and eliminate waste, namely urine.
In order to function properly, the human body extracts nutrients from food and uses them to produce energy and repair damages. Once food has been broken down and the body has retrieved what it needs, waste products stay behind in the bowel and the blood until they are removed via the urinary system. Successfully ridding the body of waste is essential to maintaining optimal health. That’s the job of the urinary system: Its construction is relatively simple, but the processes that occur within it are complex and vital to health and well-being.
Reabsorption Moves Nutrients And Water Back Into The Bloodstream
The glomerulus filters water and small solutes out of the bloodstream. The resulting filtrate contains waste, but also other substances the body needs: essential ions, glucose, amino acids, and smaller proteins. When the filtrate exits the glomerulus, it flows into a duct in the nephron called the renal tubule. As it moves, the needed substances and some water are reabsorbed through the tube wall into adjacent capillaries. This reabsorption of vital nutrients from the filtrate is the second step in urine creation.
Also Check: Pineapple Juice Kidney Stones
The Purpose Of Secretion
Often, secreted substances act as short- or long-distance signals to another cell or tissue type. For examples, neurons secrete neurotransmitters to send a message to neighboring neurons, whereas the pituitary gland secretes several types of hormones that travel via the bloodstream to act throughout the body. These types of long-distance signals can have diverse functions, including on reproductive organs, kidney function, and metabolism.
In other cases, secreted substances play a crucial functional role within an organ or tissue type. In the stomach, for example, gastric glands contain three different cell types that secrete components of gastric acid. The mucous cells secrete lubricating mucus, parietal cells secrete hydrochloric acid, and chief cells secrete the precursor to the protein-digesting enzyme, pepsin. These all work in concert to break down food inside the stomach.
Where Does Urine Go After It Passes Through The Kidneys
The urine flows out of the nephron tubule into a collecting duct. It passes out of the kidney through the renal pelvis, into the ureter, and down to the bladder. 5. Urine Is 95% Water The nephrons of the kidneys process blood and create urine through a process of filtration, reabsorption, and secretion.
Also Check: Can Kidney Stones Cause High Blood Sugar
Kidney Disease And Renal Tubular Transporters
It is currently known that preserved residual diuresis is related to better clinical outcomes than anuria in dialysis patients, since the former retains active PT transport processes.3 These transport processes are effective in removing highly protein-bound toxins, which are not adequately removed by conventional dialysis . Thus, current data suggest that renal excretion mechanism of uremic toxins is predominantly not by GFR but rather by active PT secretion.1,3 However, if OAT down-regulation observed in kidney insufficiency patients and animal models indicates a PT cells adaptation to reduce the intracellular retention of, and cellular damage from, uremic toxins, thus the increased toxin clearance by artificial OAT up-regulation could be followed by increased PT cell death from toxic exposure and residual renal function diminution.14 In acute and chronic kidney injury animal models, the uptake transporter is down-regulated since polyamine uremic toxins, such as putrescine, spermine, cadaverine, spermidine, and polyamine breakdown product , and the guanidino compounds , caused inhibition of OCT2-mediated transport.3 However, it is worth pointing out that not all tubular transporters suffer same changes in renal failure patients, since basolateral OATP4C1 expression is decreased, multidrug resistance-associated protein 2 is increased, and P-glycoprotein suffers no change.3,4
Difference Between Secretion And Excretion
Secretion vs Excretion
Both excretion and secretion involve the movement of materials in the animal body, but they are different in many ways. Both processes are very important to maintain homeostasis of the animal body. Homeostasis is maintaining of relatively constant internal body conditions, different from their external environment. These two important processes exist in single celled organisms to most advanced animals. In complex organisms, certain organs have developed for the excretion and secretion. Some organs are capable of doing both excretion and secretion processes .
What is Secretion?
Secretion is the process of releasing and transporting a specific chemical substance from one place to another. The substances are normally released from a cell or gland in animals. In prokaryotes, since they do not have specific glands, secretion means the translocation of specific molecules from a bacterial cell to its exterior via the plasma membrane.
What is Excretion?
Excretion is a vital process in all forms of life. It involves the removal of metabolic waste from the animal body, and it balances the water and salt. Excretion also maintains proper concentrations of dissolved substances and water in the cells and fluids of organisms. In prokaryotes, waste products are simply discharged through their cell membrane, but multicellular animals have evolved more complex excretory methods with complexity of their body structure.
Read Also: What Side Is Your Kidneys On
Tubular Secretion Markers Glomerular Filtration Rate Effective Renal Plasma Flow And Filtration Fraction In Healthy Adolescents
- Jesse C. SeegmillerCorrespondenceAddress for Correspondence: Jesse C. Seegmiller, PhD, DABCC, Laboratory Medicine and Pathology, University of Minnesota, 420 Delaware St SE, Mayo Bldg, Rm D185, Minneapolis, MN 55455.Advanced Research and Diagnostic Laboratory, University of Minnesota, Minneapolis, MNDepartment of Laboratory Medicine and Pathology, University of Minnesota, Minneapolis, MN
- Division of Nephrology-Hypertension, Department of Medicine, University of California San Diego, San Diego, CANephrology Section, Medicine Service, Veterans Affairs San Diego Healthcare System, La Jolla, CADivision of Preventive Medicine, Department of Preventive Medicine and Public Health, University of California San Diego, San Diego, CA
- AffiliationsSection of Endocrinology, Department of Pediatrics, University of Colorado School of Medicine, Aurora, CODivision of Renal Diseases and Hypertension, Department of Medicine, University of Colorado School of Medicine, Aurora, CO
pKidney Int.
Kidney Int.
| Measurement |
|---|
Where Does Reabsorption And Secretion Take Place In The Kidney
distal tubuleRegulated reabsorption, in which hormones control the rate of transport of sodium and water depending on systemic conditions, takes place in the distal tubule and collecting duct. Even after filtration has occured, the tubules continue to secrete additional substances into the tubular fluid.
Don’t Miss: Std That Causes Kidney Pain
Regulation Of Blood Pressure
Another function of the kidneys is to help regulate the body’s blood pressure by excreting excess sodium. If too little sodium is excreted, blood pressure is likely to increase. The kidneys also help regulate blood pressure by producing an enzyme called renin. When blood pressure falls below normal levels, the kidneys secrete renin into the bloodstream, thereby activating the renin-angiotensin-aldosterone system Regulating Blood Pressure: The Renin-Angiotensin-Aldosterone System High blood pressure is persistently high pressure in the arteries. Often no cause for high blood pressure can be identified, but sometimes it occurs as a result of an underlying… read more , which in turn raises blood pressure. The kidneys also produce urotensin, which causes blood vessels to constrict and helps raise blood pressure. A person with kidney failure is less able to regulate blood pressure and tends to have high blood pressure.
Where Does Reabsorption Of Magnesium Occur In The Kidney
Reabsorption in the distal tubule and collecting duct: The tubular fluid now enters the distal tubule and collecting duct, or terminal nephron. Reabsorption of magnesium differs in that the majority of the reabsorption occurs in the ascending limb of the loop of Henle. Where does osmosis occur in the kidney?
Recommended Reading: Orange Juice Renal Diet
Where Does Renal Reabsorption Occur
proximal convoluted tubuleWith up to 180 liters per day passing through the nephrons of the kidney, it is quite obvious that most of that fluid and its contents must be reabsorbed. Reabsorption occurs in the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and to a lesser degree, the collecting ducts.
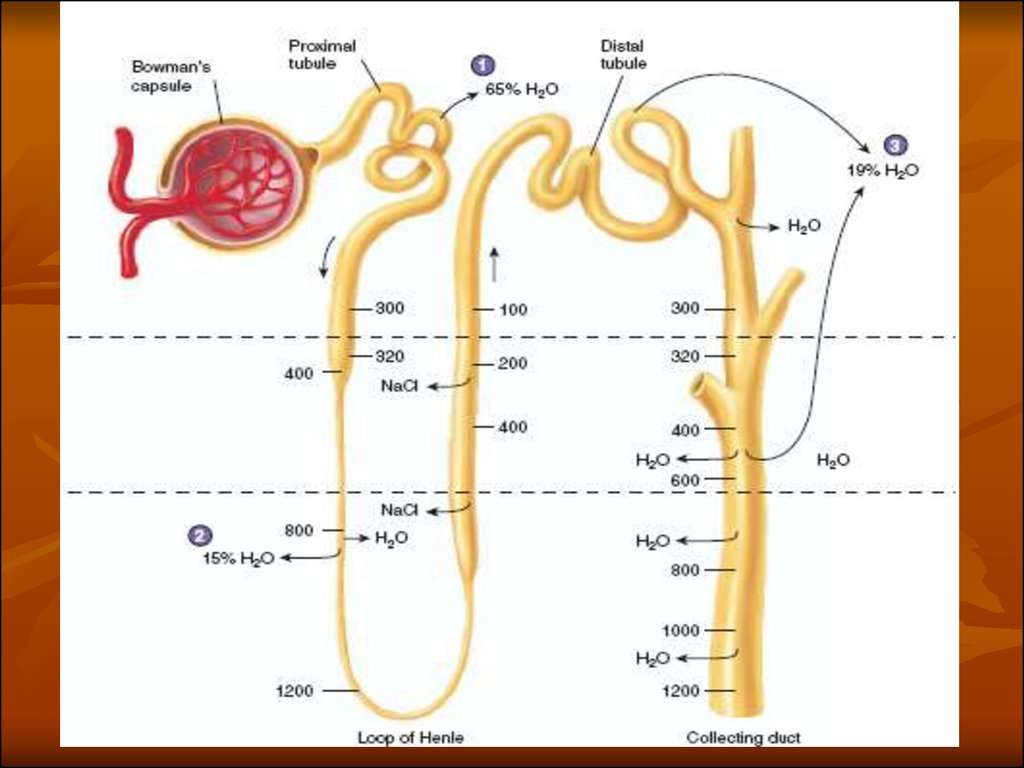
Water Reabsorption Distal And Collecting Tubules 1
Water reabsorption in the distal convoluted tubules and the collecting ducts depends on the permeability of the tubules to water, and the osmotic pressure of the interstitial fluid surrounding the tubules.
The function of the EARLY distal convoluted tubule differs from that of the last third, called the LATE distal tubule.
The late distal tubule and the collecting tubules are made permeable to water by the presence in the circulation of antidiuretic hormone released from the posterior pituitary gland . The early distal tubule is not permeable to water and its permeability is not changed by ADH.
The osmotic pressure of the interstitial fluid which surrounds the tubules throughout the cortex is isosmotic or the clinical term isotonic . In the medulla there is a gradient of osmotic pressure in the interstitial fluid. It increases from 300 mosmol/kg H2O at the cortico-medullary junction to 1400 mosmol/kg H2O at the tip of the papilla. The gradient is formed by the counter-current mechanism in the loops of Henle .
When ADH is PRESENT in circulation:
ADH increases intracellular cAMP which causes the insertion of water channels into the membrane of the cells, making them permeable to water.
Gerhard Burckhardt, Hermann Koepsell, in, 2008
You May Like: Is Watermelon Good For Your Kidneys
The Proximal Tubule Reabsorbs An Isosmotic Solution
The reabsorption of nutrients, water, and salt from the proximal tubule was described in Chapter 7.4 and is summarized again in Figure 7.5.2. The Na+,K+-ATPase provides the motive force for all of the cotransport processes by establishing a favorable electrochemical gradient for Na+ entry into the cell at the apical membrane. This favorable gradient powers the movement of a large number of solutes including glucose, amino acids, phosphate, lactate, sulfate, and indirectly through Na+H+ exchange, HCO 3 . Water and urea reabsorption passively follow the movement of osmotically active solutes so that the fluid that remains at the end of the proximal tubule is isosmotic with plasma. At this point, all of the nutrients are reabsorbed but the concentration of some secreted materials is higher. This fluid is presented to the loop of Henle.
David A. Rubenstein, … Mary D. Frame, in, 2012
What Is Secretion In The Kidney
secretionrenalreabsorptionsecretiontransportsecreted
. In this manner, where does secretion occur in the kidney?
Secretion. Secretion , which occurs in the proximal tubule section of the nephron , is responsible for the transport of certain molecules out of the blood and into the urine.
Similarly, what is reabsorption in the kidney? In renal physiology, reabsorption or tubular reabsorption is the process by which the nephron removes water and solutes from the tubular fluid and returns them to the circulating blood. Substances are reabsorbed from the tubule into the peritubular capillaries.
Also asked, what is the difference between secretion and excretion in the kidney?
Trick to Remember the DifferenceBoth of these words refer to the production of biological substances by the body. The main difference is that the products of excretion are waste, like feces or urine. The products of secretion perform other functions for the body, like lubrication, protection, or cleaning.
What is secretion in urine formation?
Waste Ions and Hydrogen Ions Secreted from the Blood Complete the Formation of Urine. At the same time, waste ions and hydrogen ions pass from the capillaries into the renal tubule. This process is called secretion. The secreted ions combine with the remaining filtrate and become urine.
Read Also: Is Celery Juice Good For Your Kidneys
What Is The Process Of Urine Formation
4.2/5Steps of Urine Formationurinesteps of urine formation
Also know, how is urine formed?
Urine is formed in the kidneys through a filtration of blood. The urine is then passed through the ureters to the bladder, where it is stored. During urination, the urine is passed from the bladder through the urethra to the outside of the body.
Also, how is urine formed Class 10? Urine is formed in three main steps- glomerular filtration, reabsorption and secretion. It comprises 95 % water and 5% wastes such as ions of sodium, potassium and calcium, and nitrogenous wastes such as creatinine, urea and ammonia. Osmoregulation is the process of maintaining homeostasis of the body.
Beside this, what are the three stages of urine formation and where do they occur?
It is primarily composed of water and urea. Urea is a special nitrogenous waste compound that the body must routinely remove. Urine formation occurs in the kidney in three stages: filtration, reabsorption, and secretion.
How is dilute urine formed?
Formation of dilute urine depends on decreased secretion of ADH from pituitary. Urine ? ADH increases the permeability of the distal tubules & collecting ducts to water. ? Highly osmolar renal medullary interstitium provides osmotic gradient for water reabsorption in presence of ADH.
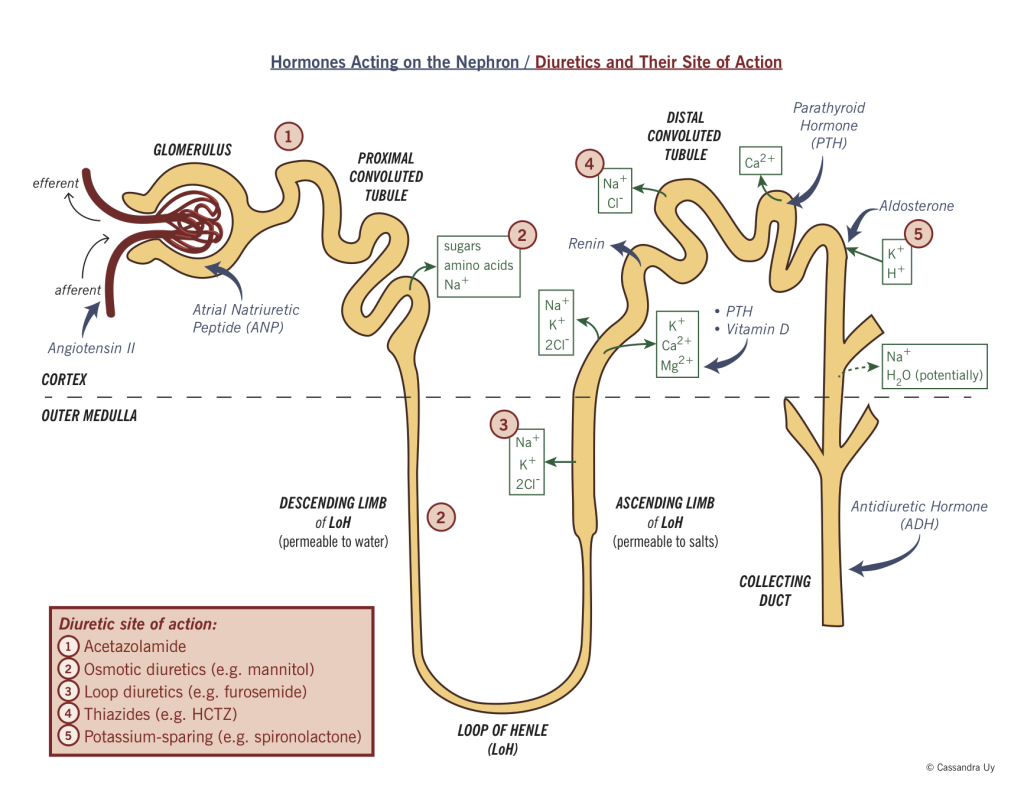
Regulation Of Water And Electrolyte Balances
Hormones control tubular reabsorption to regulate body fluid volumes and solute concentrations. A hormone is a substance that is secreted from an endocrine gland or gonad and transported through the blood to the site of action. Aldosterone acts on the collecting tubule and duct cells to increase Na+ reabsorption and H+ and K+ secretion. Angiotensin II acts on the proximal, distal, and collecting tubule cells to increase Na+ reabsorption and H+ secretion. ADH acts on the collecting tubule and collecting duct cells to increase water and urea reabsorption .
Joseph Feher, in, 2017
Also Check: Is Pomegranate Juice Good For Your Kidneys
Processes Of The Kidneys
Filtration
Filtration is the mass movement of water and solutes from plasma to the renal tubule that occurs in the renal corpuscle. About 20% of the plasma volume passing through the glomerulus at any given time is filtered. This means that about180 liters of fluid are filtered by the kidneys every day. Thus, the entire plasma volume is filtered 60 times a day! Filtration is primarily driven by hydraulic pressure in the capillaries of the glomerulus.
Note that the kidneys filter much more fluid than the amount of urine that is actually excreted . This is essential for the kidneys to rapidly remove waste and toxins from the plasma efficiently.
Reabsorption
Reabsorption is the movement of water and solutes from the tubule back into the plasma. Reabsorption of water and specific solutes occurs to varying degrees over the entire length of the renal tubule. Bulk reabsorption, which is not under hormonal control, occurs largely in the proximal tubule. Over 70% the filtrate is reabsorbed here. In addition, many important solutes are actively transported out of the proximal tubule such that their concentrations are normally extremely low in the remaining fluid. Further bulk reabsorption of sodium occurs in the loop of Henle.
Regulated reabsorption, in which hormones control the rate of transport of sodium and water depending on systemic conditions, takes place in the distal tubule and collecting duct.
Secretion
Excretion