What Are Clinical Trials And Are They Right For You
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
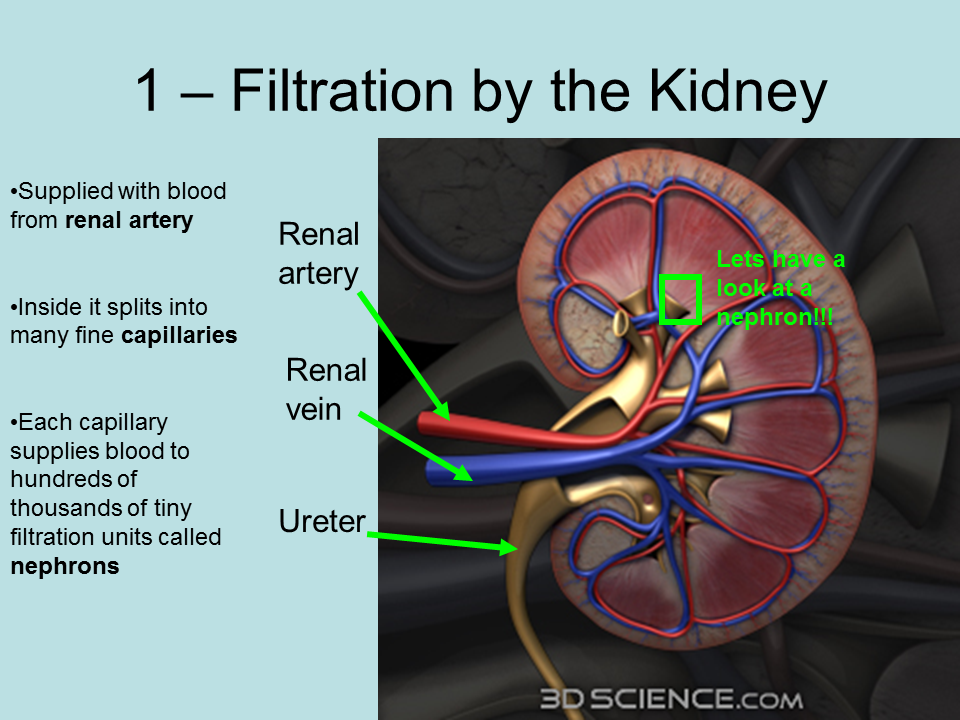
Renal Pelvis And Ureter
Numerous collecting ducts merge into the renal pelvis, which then becomes the ureter. The ureter is a muscular tube, composed of an inner longitudinal layer and an outer circular layer. The lumen of the ureter is covered by transitional epithelium . Recall from the Laboratory on Epithelia that the transitional epithelium is unique to the conducting passages of the urinary system. Its ability to stretch allows the dilation of the conducting passages when necessary. The ureter connects the kidney and the urinary bladder.
True Gfr Inulin Clearance
Inulin is a large carbohydrate polymer that lacks the one defect of creatinine. After filtration the nephron cells neither reabsorb it back into the blood nor secrete it from blood into the tubule fluid. It passes as through a glass tube. So the clearance of inulin is GFR.
Given this perfect marker, how bad a marker is creatinine?
Jacob Lemann, a great scientist and a close friend, left behind at his death the lab books of his experiments. We had the good fortune to get copies made, page by page. From these we copied out multiple instances where he measured both inulin and creatinine clearances. I made this graph to compare them.
First, take a look at the axes. GFR values are in hundreds of ml/min. Five ml fill a teaspoon, 15 ml fill a tablespoon, 30 ml is a shot of whiskey. The two kidneys can filter a lot out of blood every minute, enough to fill 3 4 shot glasses, or more.
The diagonal line marks a one to one correspondence. Most of the points lie above it. This reflects the secretion of creatinine by OAT-1. CCr overestimates GFR. But CCr moves in parallel with the true GFR and therefore is useful.
The dashed reference lines lie at the medians for inulin and creatinine clearance . As an estimate, therefore, CCr overestimates CIn by about 128/112 or 11%. That overestimate from secretion is clearly due to a constant secretion acting as the intercept of the linear regression of CCr on Cin.
Don’t Miss: How To Improve Kidney Function
Glomerular Filtration Rate Test
What is a glomerular filtration rate test?
Your kidneys are your bodys main filtration system. They remove waste products from your blood and excrete them via your urine. Glomeruli are the small filters inside your kidneys. If your kidneys arent working properly, your glomeruli wont filter as efficiently. Your doctor may order a glomerular filtration rate test if they suspect your kidneys arent working properly. This is a simple blood test.
How Do My Kidneys Work
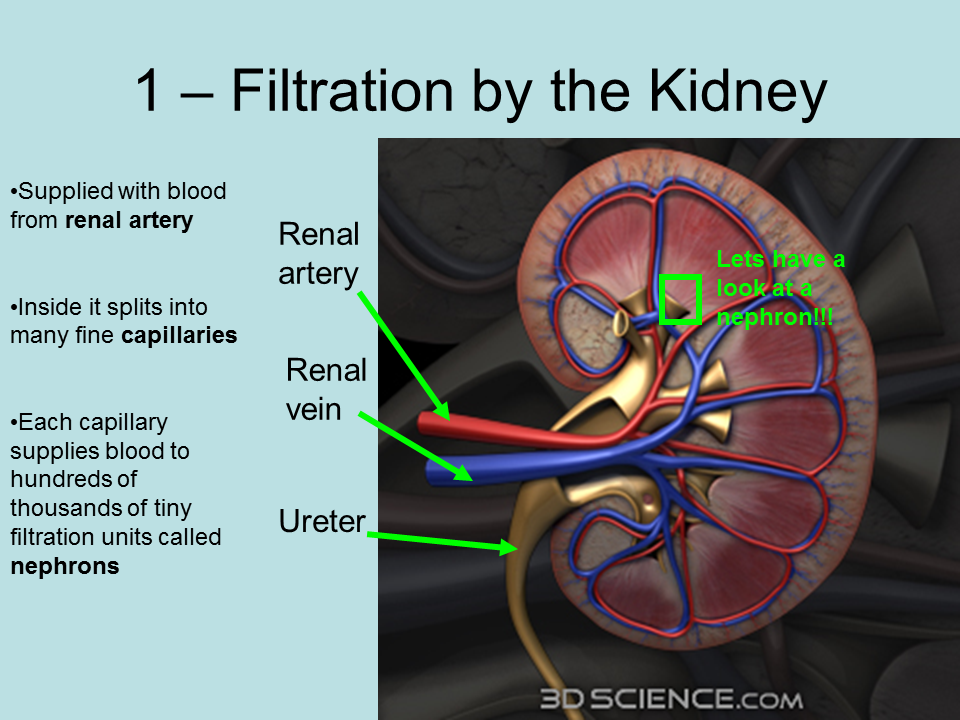
Each of your kidneys is made up of about a million filtering units called nephrons. Each nephron includes a filter, called the glomerulus, and a tubule. The nephrons work through a two-step process: the glomerulus filters your blood, and the tubule returns needed substances to your blood and removes wastes.
Don’t Miss: How To Save Kidneys Naturally
What Clinical Trials Are Open
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health. The NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
Why The Test Is Performed
The GFR test measures how well your kidneys are filtering the blood. Your doctor may order this test if there are signs that your kidneys are not working well. It may also be done to see how far kidney disease has progressed.
The GFR test is recommended for people with chronic kidney disease. It is also recommended for people who may develop kidney disease due to:
- Family history of kidney disease
- Frequent urinary tract infections
- Urinary blockage
Don’t Miss: Do Kidney Stones Affect Sperm
Fenestrated Capillaries As Primary Portals Of Renal Filtration
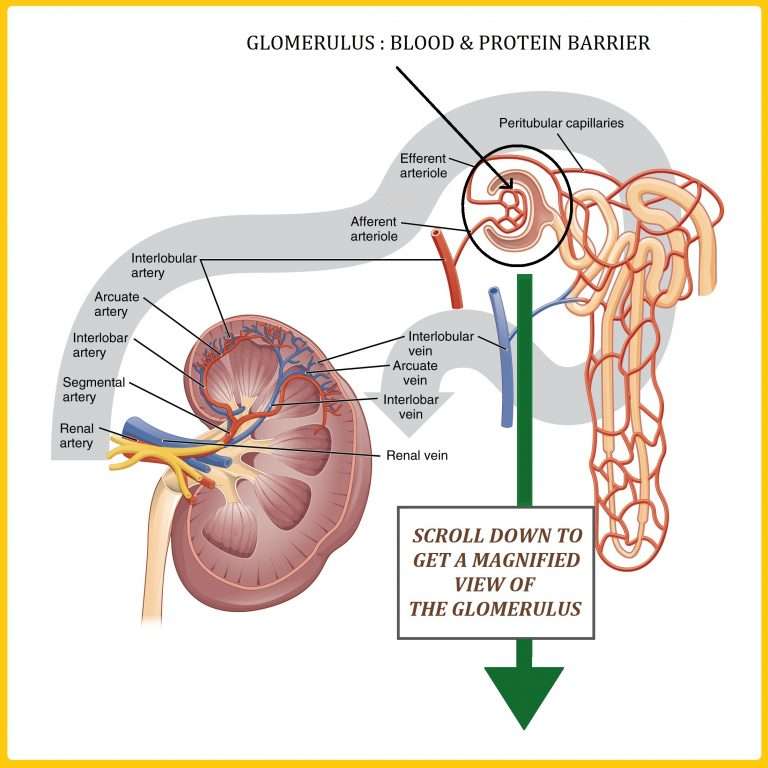
The glomerular vasculature consists of afferent and efferent arterioles and the glomerular capillary tuft . Blood enters and exits the glomerulus via the afferent and efferent arterioles, respectively. Inside the glomerulus, the afferent arteriole immediately branches into the elaborate glomerular capillary tuft, a specialized region where blood filters through. Unlike the afferent and efferent arterioles, the glomerular capillaries are heavily perforated with transcellular pores and are not surrounded by smooth muscles. These glomerular capillary pores, known as fenestrae , are 60100 nm wide and comprise 20% of the endothelial surface, making glomerular capillaries efficient portals for the rapid passage of high volumes of fluid characteristic of renal filtration .
Application of correlative STORM imaging to kidneys of Alport mice demonstrates the dramatic redistribution of agrin and 112 collagen into a diffuse pattern throughout the width of the GBM. A likely implication of this is that podocytes might be inappropriately exposed to type IV collagens, thereby inducing a pathological transformation as observed in Alport disease. These imaging analyses bolster the argument that the ultrafine pore structure of the GBM is key to normal filtration, and that proteinuria results from perturbing the molecular and structural organization of the GBM.
Pathophysiology Of Fluid Retention In Cirrhosis
In cirrhosis, disturbances in fluid balance precede ascites formation by several weeks. In this phase, intravascular volume expansion results from renal sodium retention.140 Renal tubular sodium retention also precedes changes in renal blood flow, GFR, filtration fraction, and intrarenal vascular resistance associated with cirrhosis.127 A 36% plasma volume expansion occurred in cirrhotic dogs during this active salt-retaining, preascitic phase, with two thirds of the newly acquired volume distributed to the vasodilated splanchnic circulation.126 Ascites formation is hastened by sodium ingestion or intravenous administration of sodium-containing fluids. Surgical creation of portosystemic shunting in dogs with hepatic cirrhosis abolished portal hypertension and the early tendency for renal sodium retention and ascites. In such studies, 20- to 30-lb cirrhotic dogs with shunts were able to maintain normal sodium balance with intakes as high as 85 mEq/day. Cirrhotic dogs without shunts accumulated sodium at this level of intake.225
Peripheral arterial and splanchnic vasodilatation initiates water and sodium conservation in cirrhosis.90 Peripheral arterial vasodilatation reenforces the signal initiating renal sodium retention . The physiologic responses observed after acute portal vein constriction are similar to those associated with the hyperdynamic circulatory syndrome of cirrhosis.21
Read Also: Is Maize Good For Kidney Patients
Tubular Reabsorption And Secretion
Tubular reabsorption occurs in the PCT part of the renal tubule. Almost all nutrients are reabsorbed, and this occurs either by passive or active transport. Reabsorption of water and some key electrolytes are regulated and can be influenced by hormones. Sodium is the most abundant ion and most of it is reabsorbed by active transport and then transported to the peritubular capillaries. Because Na+ is actively transported out of the tubule, water follows it to even out the osmotic pressure. Water is also independently reabsorbed into the peritubular capillaries due to the presence of aquaporins, or water channels, in the PCT. This occurs due to the low blood pressure and high osmotic pressure in the peritubular capillaries. However, every solute has a transport maximum and the excess is not reabsorbed.
In the loop of Henle, the permeability of the membrane changes. The descending limb is permeable to water, not solutes the opposite is true for the ascending limb. Additionally, the loop of Henle invades the renal medulla, which is naturally high in salt concentration and tends to absorb water from the renal tubule and concentrate the filtrate. The osmotic gradient increases as it moves deeper into the medulla. Because two sides of the loop of Henle perform opposing functions, as illustrated in Figure 22.8, it acts as a countercurrent multiplier. The vasa recta around it acts as the countercurrent exchanger.
Recommended Reading: Can Wine Cause Kidney Stones
Measuring How Your Kidneys Work
It is difficult to calculate the exact rate at which your kidneys work. The best measure of kidney function is called the glomerular filtration rate . The GFR can be estimated using a mathematical formula. This formula uses the level of creatinine in your blood to estimate how well your kidneys are filtering waste from your blood. It can indicate if there is any kidney damage.
The higher the filtration rate, the better the kidneys are working. A GFR of 100 mL/min/1.73 m2 is in the normal range. This is about equal to 100 per cent kidney function. Based on this measurement system, a GFR of 50 mL/min/1.73 m2 could be called 50 per cent kidney function and a GFR of 30 mL/min/1.73 m2 could be called 30 per cent kidney function.
If your doctor orders a blood test to learn more about your kidney function, an eGFR result is provided automatically, along with your creatinine results.
Your doctor may also test for other signs and conditions that may indicate you have chronic kidney disease. These may include tests for:
- protein in your urine
- blood in your urine
- high blood pressure
- diabetes.
Recommended Reading: What Does The Medulla In The Kidney Do
How Do You Calculate The Filtration Fraction
The is the ratio between the and . A healthy individual has a GFR of around 120 ml/min and an RPF of around 600 ml/min. This results in a FF of 0.2 or 20%. The remaining 80% of renal plasma flow will then be part of the pericapillary surrounding the renal tubules after leaving the glomerular capillaries.
Join millions of students and clinicians who learn by Osmosis!
Why Are The Kidneys Important
Your kidneys remove wastes and extra fluid from your body. Your kidneys also remove acid that is produced by the cells of your body and maintain a healthy balance of water, salts, and mineralssuch as sodium, calcium, phosphorus, and potassiumin your blood.
Without this balance, nerves, muscles, and other tissues in your body may not work normally.
Your kidneys also make hormones that help
Watch a video about what the kidneys do.
Read Also: What Is Polycystic Kidney Disease
How Much Filtrate Is Produced By The Kidneys Each Day
About 20% of the plasma volume passing through the glomerulus at any given time is filtered. This means that about 180 liters of fluid are filtered by the kidneys every day.
How is glomerular filtrate formed?
Filtrate is produced by the glomerulus when the hydrostatic pressure produced by the heart pushes water and solutes through the filtration membrane. The volume of filtrate formed by both kidneys per minute is termed glomerular filtration rate .
Waste Ions And Hydrogen Ions Secreted From The Blood Complete The Formation Of Urine
The filtrate absorbed in the glomerulus flows through the renal tubule, where nutrients and water are reabsorbed into capillaries. At the same time, waste ions and hydrogen ions pass from the capillaries into the renal tubule. This process is called secretion. The secreted ions combine with the remaining filtrate and become urine. The urine flows out of the nephron tubule into a collecting duct. It passes out of the kidney through the renal pelvis, into the ureter, and down to the bladder.
You May Like: Why Do We Need Kidneys
Applications Of Ultrafiltration Principle
- The ultrafiltration principle is used in hemodialysis machines which are used when blood pressure is more than the dialysate pressure. This process helps to separate fluid from blood without disturbing the blood cells.
- Slow Continuous Ultrafiltration is a renal replacement therapy that is based on the principle of ultrafiltration. The therapy is used to remove fluid continuously for patients with kidney failure.
- The principle of ultrafiltration is also used in chemical, pharmaceutical, manufacturing industries as well as for wastewater management.
Regulation Of Blood Pressure
Another function of the kidneys is to help regulate the bodyâs blood pressure by excreting excess sodium. If too little sodium is excreted, blood pressure is likely to increase. The kidneys also help regulate blood pressure by producing an enzyme called renin. When blood pressure falls below normal levels, the kidneys secrete renin into the bloodstream, thereby activating the renin-angiotensin-aldosterone system Regulating Blood Pressure: The Renin-Angiotensin-Aldosterone System High blood pressure is persistently high pressure in the arteries. Often no cause for high blood pressure can be identified, but sometimes it occurs as a result of an underlying⦠read more , which in turn raises blood pressure. The kidneys also produce urotensin, which causes blood vessels to constrict and helps raise blood pressure. A person with kidney failure is less able to regulate blood pressure and tends to have high blood pressure.
Also Check: Can A Ct Scan Without Contrast Detect Kidney Cancer
Module : The Urinary System
- Describe the process of filtration and relate it to net filtration pressure.
The process of producing urine occurs in three stages: filtration, reabsorption, and secretion. The physiologic goal is to modify the composition of the blood plasma and, in doing so, eliminate only waste in the form of urine.
Why Do We Care
Stones may injure kidneys as they obstruct. Surgery may injure kidneys. Kidneys can be lost. So kidney stone patients can lose kidney function. Estimating equations are a clue. If coupled with blood, the 24 hour kidney stone testing will show true creatinine clearance. But that, though in one way more exact than CKD EPI, overestimates true GFR in another creatinine secretion. Most of the time all of the measures will coincide well enough for routine care. Definitive measurements like inulin clearance are not clinically feasible.
Don’t Miss: Can Your Kidneys Fail From Alcohol
Autoregulatory Behavior At The Single Nephron Level
These results have indicated that interruption of distal delivery leads to increases in SNGFR which are presumably due to feedback mediated arteriolar vasodilation and associated increases in glomerular pressure and glomerular plasma flow. This interpretation suggests that interruption of distal volume delivery also interferes with autoregulation of glomerular pressure. Studies using the stop flow pressure technique to estimate glomerular pressure have demonstrated that glomerular pressure in nephrons with interrupted distal delivery fails to exhibit appropriate autoregulatory behavior even under conditions of coincident whole kidney autoregulation . These data support the interpretation that the general inability to autoregulate SNGFR during interrupted distal delivery is due, in part, to an associated impairment of glomerular pressure autoregulation.
Janice B. Schwartz MD, in, 2004
Capillary Network Within The Nephron
The capillary network that originates from the renal arteries supplies the nephron with blood that needs to be filtered. The branch that enters the glomerulus is called the afferent arteriole. The branch that exits the glomerulus is called the efferent arteriole. Within the glomerulus, the network of capillaries is called the glomerular capillary bed. Once the efferent arteriole exits the glomerulus, it forms the peritubular capillary network, which surrounds and interacts with parts of the renal tubule. In cortical nephrons, the peritubular capillary network surrounds the PCT and DCT. In juxtamedullary nephrons, the peritubular capillary network forms a network around the loop of Henle and is called the vasa recta.
Donât Miss: Is Watermelon Good For Kidney Patients
Recommended Reading: Can Taking Creatine Cause Kidney Problems
Blood Filtration In The Kidney
The kidneys filter about one-quarter of the blood that is output by the heart daily. This blood is sent to the bodys filter treatment plant, where it is purified by the kidneys and circulated on to the rest of the body. Some of the blood flow becomes fluid waste and is sent into the bladder for storage until it can be conveniently expelled. This toxic waste is called urine.
The paired kidneys in the upper part of the abdomen toward the back Continue Scrolling To Read More Below…
Feature: Human Biology In The News
Kidney failure is a complication of common disorders including diabetes mellitus and hypertension. It is estimated that approximately 12.5% of Canadians have some form of kidney disease. If the disease is serious, the patient must either receive a donated kidney or have frequent hemodialysis, a medical procedure in which the blood is artificially filtered through a machine. Transplant generally results in better outcomes than hemodialysis, but demand for organs far outstrips the supply. The average time on the organ donation waitlist for a kidney is four years. There are over 3,000 Canadians on the wait list for a kidney transplant and some will die waiting for a kidney to become available.
For the past decade, Dr. William Fissell, a kidney specialist at Vanderbilt University, has been working to create an implantable part-biological and part-artificial kidney. Using microchips like those used in computers, he has produced an artificial kidney small enough to implant in the patients body in place of the failed kidney. According to Dr. Fissell, the artificial kidney is a bio-hybrid device that can mimic a kidney to remove enough waste products, salt, and water to keep a patient off dialysis.
Don’t Miss: Can Kidneys Start Working Again After Dialysis
Why Red Blood Cells Are Normally Absent From Glomerular Filtrate
The filtrate does not contain proteins and blood cells as they are too large for the pores. 2. Selective reabsorption: Reabsorption of useful substances e.g. water, amino acids, glucose, vitamins and salts from glomerular filtrate back into capillaries.
What molecules are found in filtrate?
Glomerular filtrate contains a lot of water, but also important molecules like glucose, amino acids, salts and excretory material, urea.
In which part of the kidney is blood filtered?
Each of your kidneys is made up of about a million filtering units called nephrons. Each nephron includes a filter, called the glomerulus, and a tubule. The nephrons work through a two-step process: the glomerulus filters your blood, and the tubule returns needed substances to your blood and removes wastes.
Where are red blood cells filtered?
Modeling blood filtration The spleens primary function is to remove old red blood cells from circulation when they can no longer perform their job.
Which component of blood is not present in the glomerular filtrate?
Proteins will be present in blood plasma, but not present in glomerular filtrate or urine. This is because proteins cannot pass across the basement membrane during ultrafiltration and thus cannot form part of the filtrate.