What Happens To Patients With Calcium Metabolism Disorders
Hypercalcemia is a common disorder that can present a challenge to clinicians. The cause of hypercalcemia can either be easy or very difficult to identify. The pathophysiology and prognosis of hypercalcemia depends on the underlying cause.
In order to understand how hypercalcemia occurs it is important to know how calcium is regulated in the body. The majority of total body calcium is stored in bone. Only 1% of calcium is extracellular and serum calcium makes up only 0.1-0.2% of extracellular calcium. Forty percent of total serum calcium is free or ionized. The remaining serum calcium is protein bound, mainly to albumin. Serum levels of calcium are tightly regulated through the actions of PTH and 1,25-dihydroxyvitamin D .
PTH is a polypeptide produced by the parathyroid gland. It is stimulated through calcium sensing receptors by low ionized calcium and results in 1) increased renal absorption of calcium 2) increased mobilization of calcium from the skeleton and soft tissues and 3) increased production of 1,25-dihydroxyvitamin D and subsequent increased intestinal absorption of calcium. The increase in PTH from hypocalcemia restores serum calcium levels to normal. PTH secretion is lowered in hypercalcemia as increases in serum ionized calcium suppress PTH secretion.
Primary hyperparathyroidism
Epidemiology
Clinical presentation
Pathophysiology
Natural history
Medical therapy
Tertiary hyperparathyroidism
Epidemiology
Clinical manifestations
Pathophysiology
Natural history
What Is The Cause Of This Patient’s Calcium Metabolism Disorder
Hypercalcemia
Hypercalcemia occurs when the serum level of ionized , not total, calcium increases. It occurs when the total serum calcium level is > 10.5 mg/dL or the ionized calcium level is > 5.6 mg/dL . Hypercalcemia is a common disorder that can be a challenge to clinicians.
The two most common causes of hypercalcemia are primary hyperparathyroidism and malignancy. Together, they account for over 90% of all cases. The clinical history can help distinguish between the two disorders and can identify other less common causes of hypercalcemia . It is important to identify the cause as treatment and prognosis vary according to the underlying disorder. A careful history and physical should be performed focusing on the following key elements.
Table 1.
Causes of Hypercalcemia
Risk factors for malignancy should be evaluated in the history. Hypercalcemia is most common with hematologic malignancies and solid tumors of the breast, ovary, lung and kidney. Malignancy is usually evident clinically by the time hypercalcemia develops. Symptoms of hypercalcemia are often more severe in patients with malignancy whereas asymptomatic hypercalcemia is common in patients with primary hyperparathyroidism. The clinical manifestations of hypercalcemia are discussed below.
The history should focus on other rare causes of hypercalcemia including chronic kidney disease, immobility and the recovery phase of acute renal failure secondary to rhabdomyolysis.
Table 2.
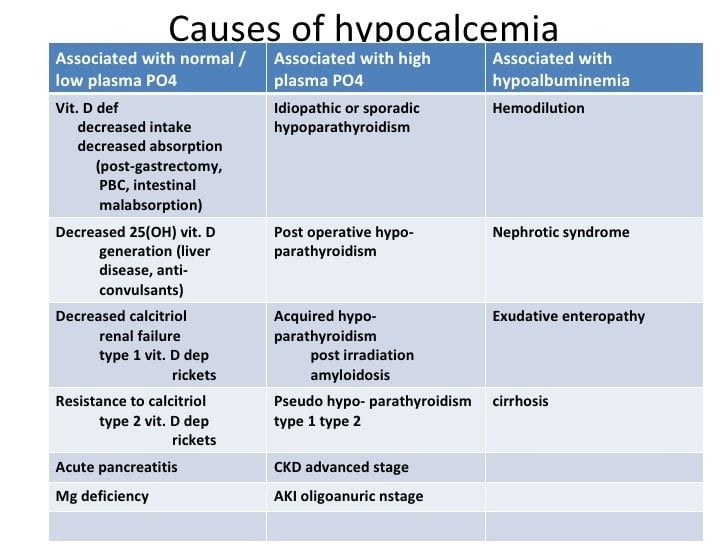
Hypocalcemia
Table 4.
How To Utilize Team Care In The Treatment Of Calcium Matabolism Disorders
Hypercalcemia
-
Specialty consultations: A nephrologist should be consulted for severe life threatening hypercalcemia as hemodialysis may be necessary. Nephrology should also be consulted for any patient with hypercalcemia and renal dysfunction. Endocrinology should be consulted if there is concern for an endocrine related etiology of the hypercalcemia. Of course, hematology/oncology should be consulted if there is a concern for malignancy related hypercalcemia.
-
Dietitians: A dietician should be consulted for patients with hypercalcemia related to excess calcium or vitamin A or D intake. Dieticians can educate patients about low calcium diets and dietary supplements.
-
Pharmacists: Pharmacists are a great resource for information on dosing and administering medications used in the treatment for hypercalcemia, especially in patients with renal failure. Pharmacists can also assist in identifying medications that result in hypercalcemia.
-
Nurses: Nurses are key in the management of acute symptomatic hypercalcemia. When saline hydration is used, urine output and vital signs must be monitored frequently. Nurses should monitor and report urine output and vital signs hourly. With close monitoring by nurses, volume overload should be prevented. Nurses should also monitor changes in symptoms, including EKG changes as more aggressive therapy may be needed if symptoms persist or worsen.
Hypocalcemia
You May Like: Does Red Wine Cause Kidney Stones
Nutritional Vitamin D Deficiency
The fortification of milk, cereals, breads, and other foods with vitamin D and the use of supplements are why there are so few cases of vitamin D deficiency in children in the United States. Vitamin D deficiency has been recognized in the United States in children who have restricted diets or specialized diets . In countries that do not fortify foods, childhood vitamin D deficiency is more common. Vitamin D deficiency is recognized as a worldwide problem in older adults as well . Exclusively breastfed infants are at high risk for vitamin D deficiency, as there is little vitamin D in human milk.
Why Does Hypocalbuminemia Cause Hypocalcemia
4.9/5HypoalbuminemiaHypoalbuminemiacausehypocalcemiaCauseshypoalbuminemia
Likewise, people ask, how does low albumin affect calcium?
Each 1 g/dL reduction in the serum albumin concentration will lower the total calcium concentration by approximately 0.8 mg/dL without affecting the ionized calcium concentration and, therefore, without producing any symptoms or signs of hypocalcemia.
Secondly, why does hypocalcemia cause paresthesia? Symptoms of hypocalcemia include signs of tetany and a pins and needles sensation or other paresthesia, which indicates neuromuscular excitation due to a lessening of the membrane-stabilizing effect normally exerted by calcium.
People also ask, how does albumin level affect calcium level?
The relationship between total serum calcium and albumin is defined by the following simple rule: the serum total calcium concentration falls by 0.8 mg/dL for every 1-g/dL fall in serum albumin concentration. This causes a decrease in the ionized calcium and may trigger symptoms of hypocalcemia.
Why do you have hypocalcemia with pancreatitis?
Pancreatitis can be associated with tetany and hypocalcemia. It is caused primarily by precipitation of calcium soaps in the abdominal cavity, but glucagon-stimulated calcitonin release and decreased PTH secretion may play a role.
Don’t Miss: Fluid Backup In Kidneys
How Is Renal Failure Treated
Early stages of renal failure are usually treated with lifestyle modifications and by controlling underlying causes such as hypertension and diabetes.
When kidney function falls below 10% of normal, the options below may be used
- Dialysis: This is a way to pump blood through a machine that filters out waste and returns the blood to the body. There are two types of dialysis
- Hemodialysis: A tube is stuck into one of the veins to remove toxins from the blood. This is usually done three times a week for three to four hours at a time.
- Peritoneal dialysis: This is done through a tube that is placed inside the belly.
Underlying Causes Leading To Hypocalcemia
Hypocalcemia can have many different potential underlying causes. Because of the key role of PTH, it is not surprising that a low level of this hormone is one of the main causes of low calcium. Some of the reasons for this include injury to the parathyroid gland from surgery or radiation treatment, autoimmune disease, or a genetic disease leading to low PTH.
Low vitamin D is also another important cause of hypocalcemia. This hormone plays an important role in your bodys ability to absorb and utilize calcium. People can have low vitamin D from a number of different problems, such as:
- Low dietary intake of vitamin D
- Little sun exposure
- Poor absorption of vitamin D
- Advanced kidney disease
- Advanced liver disease
Problems with certain blood electrolytes can also sometimes lead to hypocalcemia. For example, abnormal levels of the electrolytes magnesium and phosphate might indirectly cause hypocalcemia. Some other less common causes of hypocalcemia include pancreatitis and cancer which has spread to the bones.
A number of drugs sometimes cause hypocalcemia as a side effect. Some of these include the following:
- Certain drugs for osteoporosis
- Some antiepileptic drugs
- Certain chemotherapy drugs
- Diuretic drugs
- Proton pump inhibitors
For a variety of reasons, people who are critically ill have a higher risk of hypocalcemia. This can be due to underlying medical problems, sepsis, electrolyte problems, certain kinds of blood transfusions that affect calcium, or other factors.
Don’t Miss: Can Apple Cider Vinegar Hurt Your Kidneys
Why Can Serum Calcium Become Low In People With Kidney Disease
Our bodies can’t make vitamin D. We can only get vitamin D from food and by exposing our skin to sunlight. Healthy kidneys can take that vitamin D we absorb and change it to an active form. That active vitamin D then helps us absorb calcium.
But in chronic kidney disease , the kidneys are less able to make active vitamin D. Without enough active vitamin D, you absorb less calcium from the food you eat, so it then becomes low in your blood. Also, extra phosphorus in the blood of people with CKD may bind to calcium in the blood. This can then lower serum calcium.
A normal serum calcium level is 8.5 – 10.2 mg/dL. A serum calcium that is either too low or too high can be dangerous and both conditions need treatment. But patients with low serum calcium, even levels at the lower end of normal, have been found to reach kidney failure faster than people with higher serum calcium levels.
Clinical Presentation Of Hypocalcemia
Hypocalcemia can present as an asymptomatic laboratory finding or as a severe, life-threatening condition . Distinguishing acute from chronic hypocalcemia and asymptomatic from severely symptomatic hypocalcemia is critical for determining appropriate therapy. In the setting of acute hypocalcemia, rapid treatment may be necessary. In contrast, chronic hypocalcemia may be well tolerated, but treatment is necessary to prevent long-term complications.
Don’t Miss: Pomegranate Juice And Kidney Stones
What Can I Do To Keep My Serum Calcium Level Normal
Eat a well-balanced diet. Other nutrients such as magnesium and vitamin D are needed to absorb calcium. A dietitian who works with kidney patients can help you plan a diet that fits your individual needs. Dairy foods are high in calcium, but may also be high in phosphorus, which is usually limited in CKD. Your dietitian can help you find healthy alternatives to many high phosphorus foods.
You may need a vitamin D supplement, but your healthcare team will need to order the right one for you. Don’t take a vitamin D supplement or a calcium supplement unless your healthcare team orders one for you. If you need a medicine called a phosphate binder to lower your phosphorus, then your healthcare team may recommend one that has calcium.
Hypomagnesemia Is Often Neglected
Loss of magnesium from the GI tract and the kidneys, as well as cellular uptake, are among the causes.
CLEVELANDAlthough magnesium is abundant, it is the most neglected nutrient cation, said Zalman S. Agus, MD, at the Cleveland Clinics Nephrology Update 2008.
The effect of magnesium depletion, which causes a temporary drop in serum magnesium, is a decrease in urinary magnesium excretion. It falls and protects the serum so that while we get some magnesium depletion with a magnesium-depleted diet, the serum level doesnt fall below 1.0 mEq/L, the level at which we usually see symptoms, said Dr. Agus, emeritus professor of medicine at the University of Pennsylvania School of Medicine in Philadelphia.
Low serum magnesium causes hypocalcemia by inhibiting parathyroid hormone secretion as well as the action of PTH at the bone. Intracellular magnesium has additional effects on intracellular ion channels, activating calcium and potassium channels in both myocardial and ventricular cells and also activating chloride and potassium channels in the nephrons thick ascending limb.
The prevalence of hypomagnesemia is about 10% in community and Veterans Administration hospitals, affecting 50% of hypokalemic hospitalized patients and 60% of ICU patients.
Also Check: Can Pop Cause Kidney Stones
How Do I Know If I Have Mineral And Bone Disorder
- You will have blood tests to check your blood levels of calcium, phosphorus, PTH and vitamin D.
- Some people may need to have a bone biopsy. A bone biopsy is a sample of bone taken for study.
- Your healthcare provider may order an x-ray of your abdomen, or an echocardiogram of your heart to check if mineral imbalance has affected your heart and blood vessels.
Table 5comparison Of Features Of Pseudohypoparathyroidism And Pseudopseudohypoparathyroidism
| Gs alpha = alpha subunit of the stimulatory guanine nucleotide binding protein + = present = decreased PHP = pseudohypoparathyroidism PPHP = pseudopseudohypoparathyroidism Adapted from Juppner H and Bastepe M: Pseudohypoparathyroidism. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, C. J. Rosen , John Wiley and Sons, Eighth Edition, pp 590-600, 2013. |
In PHP 1, there is autosomal dominant inheritance of the mutation. However, there is imprinting of the GNAS locus with silencing of the paternal allele, which influences the expression of the phenotype. In PHP 1a, if the mutation is inherited from the mother, the disease in the offspring manifests as PHP 1a with low serum calcium, high serum phosphate and high PTH levels plus the presence of features of Albrightâs hereditary osteodystrophy . If the mutation is passed down from the father, that allele is silenced in the proximal tubules of the kidney . The normal sequence from the maternal allele is expressed, and the biochemical and mineral abnormalities are absent. Only the AHO phenotype is present in such an individual. This is called pseudopseudohypoparathyroidism .
Read Also: Is Pomegranate Juice Good For Kidneys
Hows Calcium Deficiency Disease Diagnosed
Contact your doctor if you have symptoms of calcium deficiency disease. Theyll review your medical history and ask you about family history of calcium deficiency and osteoporosis.
If your doctor suspects calcium deficiency, theyll take a blood sample to check your blood calcium level. Your doctor will measure your total calcium level, your albumin level, and your ionized or free calcium level. Albumin is a protein that binds to calcium and transports it through the blood. Sustained low calcium levels in your blood may confirm a diagnosis of calcium deficiency disease.
Normal calcium levels for adults can range from 8.8 to 10.4 milligrams per deciliter , according to the Merck Manual. You may be at risk for calcium deficiency disease if your calcium level is below 8.8 mg/dL. Children and teens typically have higher blood calcium levels than adults.
Hypocalcemia Is Affected In Renal Failure
Kidneys play vital role in regulating and balancing phosphorus and calcium in the blood. Kidney functions are severely damaged in renal failure that patients often have metabolic disorder of phosphorus and calcium—high serum phosphorus and low serum calcium.
Serum calcium level lower than 2.1-2.2mmol/L is called hypocalcemia. Usually patients have no obvious clinical symptoms. However if calcium concentration in the blood drops too fast or if hypocalcemia lasts for long time, it can cause serious nervous and cardiovascular lesions and in serious conditions it can be life-threatening.
There are several reasons why renal failure can cause hypocalcemia. In renal failure, the absorption of calcium in the gastrointestinal tract will decrease renal failure can cause decreased excretion of phosphorus and high phosphorus in the blood can further worsen hypocalcemia renal failure patients often have acidosis which can promote the discharge of calcium from the kidneys.
Hypocalcemia can cause osteoporosis, bone fracture and other bone problems which is very common especially among the elderly patients. Proper measures should be taken to treat hypocalcemia including treating the underlying disease, that is renal failure. Have high-calcium foods and calcium supplements if necessary. Have proper and regular exercises and have some sunshine everyday.
Also Check: Std And Kidney Pain
Derangements Of Bone Mineral Metabolism
Bone mineral metabolism and calcium-phosphorus homeostasis involve a complex interplay among kidneys, gut, bone and parathyroid glands. The metabolism involves parathyroid hormone , vitamin D and vitamin D receptors, fibroblast growth factor-23 , Klotho and calcium-sensing receptors. As regulated excretion of calcium and phosphate is carried out primarily by the kidney, kidney failure inevitably causes abnormalities in bone turnover and, in most cases, soft tissue and vascular calcification, leading to increased mortality. This triad of laboratory abnormalities, bone disorder and soft tissue calcification is collectively termed MBD .
Serum phosphorous may remain normal in most CKD patients with eGFR > 40 ml/min/1.73 m2 due to the upregulation of PTH and FGF23 and attendant inhibition of proximal tubular phosphate reabsorption . As CKD progresses, renal phosphate excretory capacity becomes exhausted, and hyperphosphatemia ensues .
What Are Calcium And Serum Calcium
Calcium is a mineral stored mainly in your bones. But it’s also found throughout the body, including the muscle and blood. You need to get calcium from your diet since the body can’t make it.
Serum calcium is the calcium in your blood.
You need calcium for these important jobs:
- Form bones and teeth
- Make muscles move , including the heart muscle
- Clot the blood to stop you from bleeding too much if you get a cut
- Help the heart keep a steady heart beat
- Help nerves work well
Calcium moves out of bones and into the blood when needed in order to keep serum calcium levels normal. If you don’t eat enough calcium, then too much comes out of the bones. When too much calcium leaves the bones, bones get weak.
If serum calcium gets too low, then enough calcium can’t go to nerves, muscles, and wounds. This can cause serious problems with the heart and other muscles, and with blood clotting.
Recommended Reading: Do Multivitamins Cause Kidney Stones
How To Manage Hypocalcemia In Kidney Failure
Kidney failure patients are running a high risk for hypocalcemia which may bring them various bone problems like bone pain and bone fracture. Hypocalcemia is the presence of low serum calcium levels in the blood and can be caused by kidney failure directly. Therefore, it is necessary for kidney disease patients to master some knowledge about how to manage hypocalcemia in kidney failure.
How does kidney failure cause hypocalcemia?
Although kidney failure is a serious illness condition regarding kidney, it always involve many other systems like digestive system, respiratory system, cardiovascular system and so on. Kidney is a bean-shaped organ with multiple function. It is responsible for keeping balance of electrolyte, so when kidney function is impaired, electrolyte disturbance occurs. Hypocalcemia is a common electrolyte problems among kidney failure patients and its occurrence is closely related with high phosphorus level in blood.
For people with kidney failure, failed kidneys can not discharge excess phosphorus, leading to high phosphorus level in blood which can affect our body and make them not get enough calcium. Therefore, for kidney failure patients who have high levels of phosphorus, they are more likely to suffer from hypocalcemia.
How to manage hypocalcemia in kidney failure?
To get hypocalcemia intro control, kidney failure patients need to:
2. Undergo calcium therapy like intravenous injection of calcium.