What Causes Low Blood Pressure
There are a number of things that can cause your blood pressure to lower to dangerous levels. Those things include:
- Taking certain medications
- Inflammation
- Shock or trauma
Shock or trauma is often the most common cause of lower blood pressure. Shock or trauma can be caused by experiencing a certain event, undergoing surgery, or certain health problems.
How The Flow Of Sodium And Potassium In The Distal Nephron Is Controlled
Increased NCC activity through WNK modulation is a final common pathway for the development of hypertension in many settings. For example, adrenergic stimulation of blood increases blood pressure by suppressing WNK4 and, in turn, increases NCC activity. Furthermore, calcineurin inhibitors are commonly used to treat autoimmune diseases and prevent transplant rejection, which often causes hypertension. Recent studies by Ellison et al have indicated that the hypertension mechanism associated with the use of calcineurin inhibitors involves the stimulation of NCC through the degradation of WNK3.
While the continued delineation of WNK functions has provided important information about renal physiology, only a small subset of patients with PHAII has a mutation in the WNK gene. Using exome sequencing, the Lifton group mutates the Kelch3 and Cullin3 genes in patients with PHAII . Furthermore, mutations in both genes cause disease in approximately 80% of individuals affected by PHAII . KLHL3 is one of a family of more than 50 Kelch proteins that contain wide-width complex Bric-a-Brax complexes, tram track, characterized by a -helix domain of six bleeds to bind specific target proteins. is. Provides scaffolding for the CUL3 complex, which includes BTB domain proteins like KLHL3 and a RING domain protein that acts as an E3 ubiquitin ligase, targeting protein substrates specific for ubiquitylation
What Is Meant By Regulation Of Kidney Function
The kidneys main function is to excrete wastes from the body. It performs other roles, like regulating blood pressure, acid-base balance, osmoregulation of electrolytes, and endocrine role. In the human body, regulation of Kidney function is very well developed. The regulation of kidneys functioning is under the control of a complex hormonal mechanism as well as the RAAS system and neural regulation. Such a control on the functioning of kidneys is called regulation of Kidney functions.
Also Check: Is Cranberry Juice Good For Your Liver And Kidneys
An Overview Of Blood Pressure Regulation Associated With The Kidney
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Immediate access to all parts of this book
- Cover-to-cover formats may be available
- Unlimited re-access via MyKarger
The final prices may differ from the prices shown due to specifics of VAT rules.
Where Are My Kidneys
The kidneys are small bean-shaped organs approximately 6 cm wide and 12 cm long and consist of two main layers an inner layer called the medulla and an outer layer called the cortex. Most people have two kidneys that are situated at the back of the abdomen on either side of the spine.
Graphic showing a section through the right kidney with the main structures labelled.
You May Like: Va Rating For Stage 3 Kidney Disease
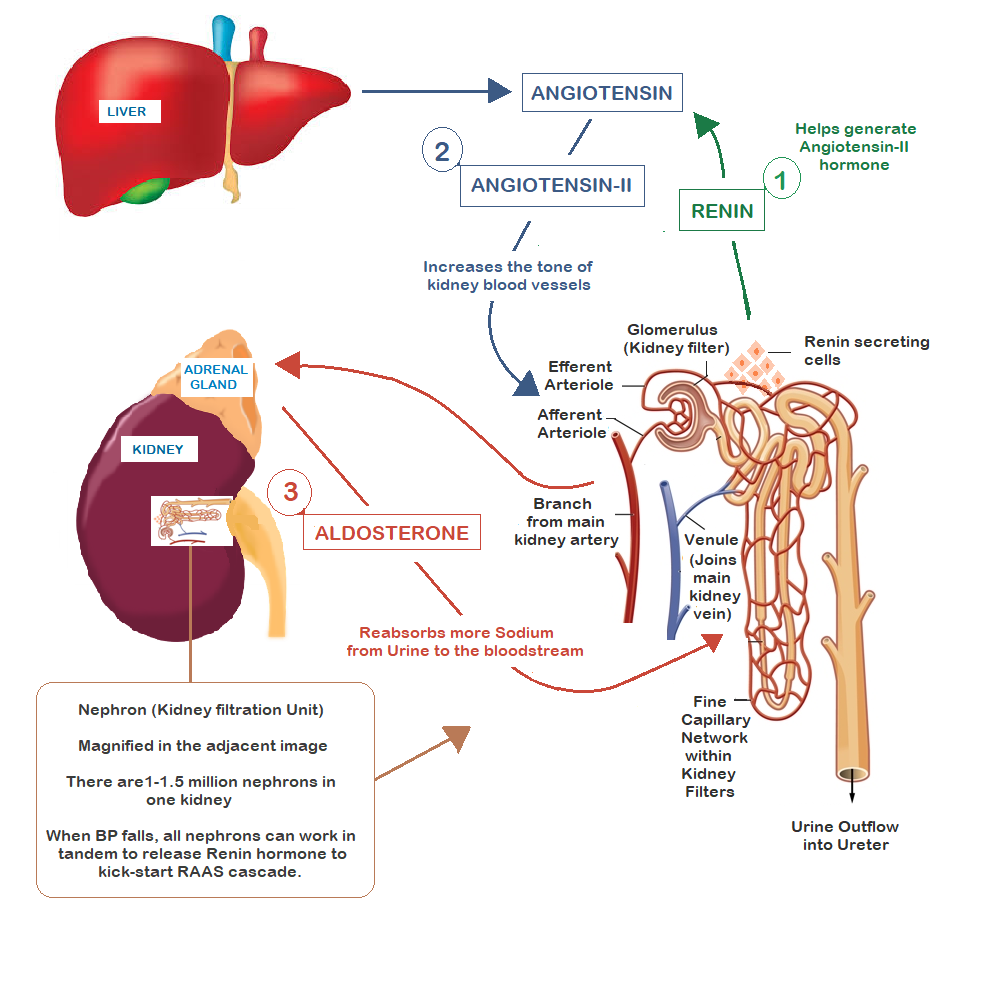
Intrarenal Actions Of The Renin
The renin-angiotensin system is a powerful modulator of blood pressure, and the reduction of RAS produces hypertension. Drug blockade of RAS with renin inhibitors, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers effectively reduces blood pressure in a substantial proportion of patients with hypertension 10 /, such as human-caused RAS. Illustrates the critical role for activation. hypertension. In rodents, the removal of the RAS gene reduces blood pressure, causing hypertension to cause hypertension .
While the cells of the distal tubule do not feel Na in the filtrate either, and the arterial cells feel the blood pressure. Studies have shown that chronic infusion of a low dose of angiotensin II directly into the kidney caused hypertension with altered nature due to a change in the pressure-natriuresis relationship.
In support of this view, recent studies have verified the critical need for ACE within the kidney, thus fully revealing the expression of the sodium transporter, renal sodium recombination, and the stimulation of hypertension in the context of RAS activation.
Fig. 1: Renal mechanism by which activation of the renin-angiotensin system reduces the ratio of pressure natriuresis and leads to hypertension .
How Does Lower Blood Pressure Cause Kidney Failure
When your blood pressure decreases it indicates that there is a change in blood flow throughout the body. A change in blood flow can cause you to experience serious problems with your kidneys. If the blood flow is not corrected, it could result in serious, potentially fatal, problems.
The kidneys are often the first organs to experience problems as a result of low blood pressure. The problems occur because there is a dramatic decrease in blood flow to the kidneys. If the kidneys dont have access to the right amount of blood, they are unable to properly filter the blood or receive enough oxygen to function. Over time these problems from the lower blood pressure result in the kidneys slowly shutting down.
Don’t Miss: What Laxative Is Safe For Kidneys
High Blood Pressure And Kidneys Symptoms
Our kidney function and blood pressure are mutually co-related. Without a steady flow of blood, the kidney cant perform very well about blood filtration. Even high circulation of blood in kidneys may lead to damage to kidneys.
It means that nephrons will perform less filtration process through its capillaries. They may even make less purification unwanted wastes, and toxic substances may get saturated in one place.
Read this 3 Painless Symptoms of Kidneys, not Filtering.
It may spread infections in the kidney as well as in the ureter duct. Also, you may see some long term series of kidney problems. As these problems, you may not find it slowly, or you cant feel anything problematic. But suddenly it appears, and your kidney will get failed within a few hours or days.
Wnk: New Routes That Regulate The Renewal Of Solute Transport
Reliable evidence showing an important role for the kidney in blood pressure regulation has defined the genetic basis for almost all Mendelian disorders associated with abnormal blood pressure phenotypes in humans. In each case, these mutations affect the recombination of sodium and liquid with nephrons. One of these disorders is type II pseudohypoaldosteronism , a Mendelian syndrome characterized by an unusual combination of hypertension and hyperkalemia, caused by a mutation in a gene encoding the WNK1 kinase . goes. WNK4. This discovery accelerated the in-depth study of these unique eunuchs, thus identifying the roles of WNK1 and WNK4 in regulating sodium and potassium flow in the distal nephron. These actions are mainly mediated by the control of the relative levels and activities of thiazide-sensitive sodium chloride cotransporters and/or renal channels of external medullary potassium . ) Through phosphorylation, whereas WNK4 De K appears to clearly target NCC for lysosomal degradation of overgrowth. .
Figure 4: Mechanisms that regulate sodium and potassium flow in distal nephrons
Read Also: Can You Have 4 Kidneys
Further Control Of Blood Pressure
Other factors that can affect long-term regulation of blood pressure are natriuretic peptides. These include:
- Atrial natriuretic peptide is synthesised and stored in cardiac myocytes. It is released when the atria are stretched and indicates high blood pressure.
- ANP acts to promote sodium excretion. It dilates the afferent arteriole of the glomerulus, increasing the glomerular filtration rate . Moreover, ANP inhibits sodium reabsorption along the nephron. Conversely, ANP secretion is low when blood pressure is low.
- Prostaglandins act as local vasodilators to increase GFR and reduce sodium reabsorption. Moreover, they act to prevent excessive vasoconstriction triggered by the RAAS and sympathetic nervous system.
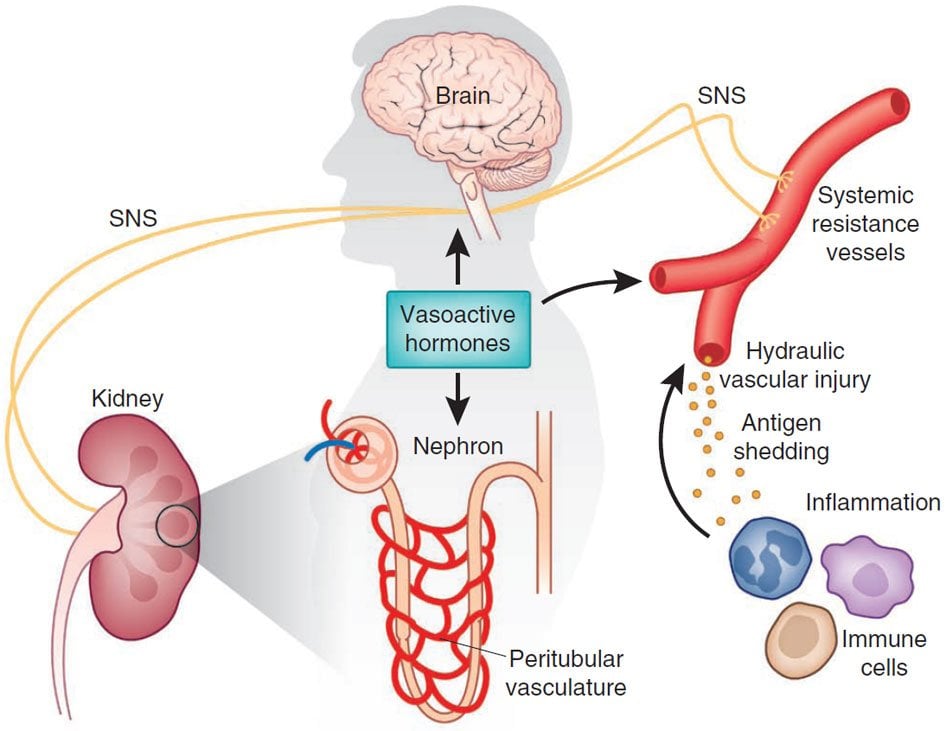
Hypertensive Kidney Injury And The Progression Of Chronic Kidney Disease
The kidney remains an important site for hypertensive organ loss, ranking second as the leading cause of End-Stage Renal Disease for diabetic nephropathy. Furthermore, the presence of chronic kidney disease , including hypertension, has been shown to be a strong independent risk factor for adverse cardiovascular outcomes. However, key aspects of clinical hypertensive kidney disease are poorly understood, such as marked differences in individual susceptibility to hypertensive kidney damage and categorical variable renoprotective effects of classes of antihypertensive drugs.
Studies have shown that time-varied SBP was associated with incident CKD, with a constant increase in incident risk CKD above SBP of 120 mmHg. Time-weighted SBP was associated with a more rapid decrease in kidney function. Diabetes was the strongest predictor of CKD, and a rapid decline in kidney function and increased glycemic control were associated with increased risk, supporting the role of BP and other traditional risk factors, such as progression of renal function in diabetes and onset and Hypertension decreases in patients with normal renal function at baseline.
Reference :
Don’t Miss: Is Mio Bad For Your Kidneys
How Blood Volume Affects Blood Pressure
Changes in blood volume affect arterial pressure by changing cardiac output. An increase in blood volume increases central venous pressure. This increases right atrial pressure, right ventricular end-diastolic pressure and volume. This increase in ventricular preload increases ventricular stroke volume by the Frank-Starling mechanism. An increase in right ventricular stroke volume increases pulmonary venous blood flow to the left ventricular, thereby increasing left ventricular preload and stroke volume. An increase in stroke volume then increases cardiac output and arterial blood pressure.
Revised 4/25/2014
DISCLAIMER: These materials are for educational purposes only, and are not a source of medical decision-making advice.
Regulation Of Blood Volume By Renal Excretion Of Water And Sodium
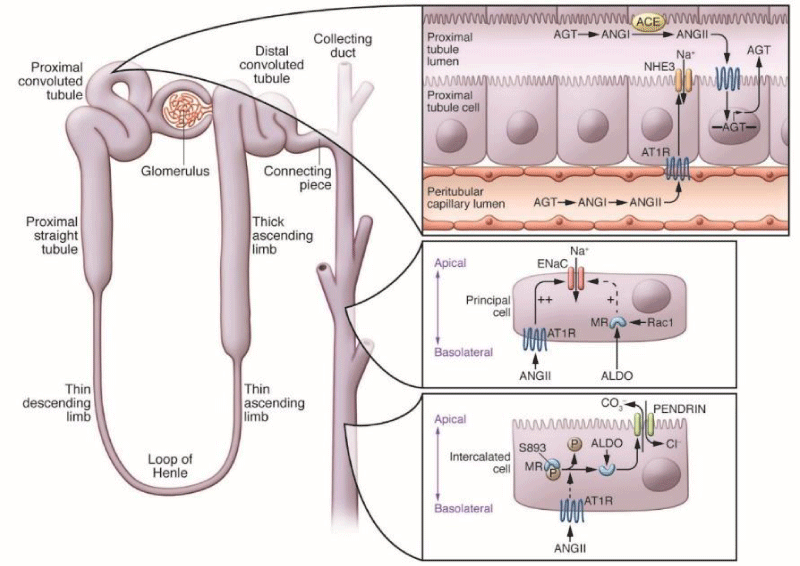
Blood is filtered at the glomerulus. This filtrate contains sodium, water and other substances. As the filtrate travels through the proximal tubule, loop of Henle, distal and collecting tubules, the concentration of sodium is altered by transport of sodium across the tubular wall and into the renal interstitium, where it can diffuse into a dense network of intrarenal capillaries. Some of the renal tubules are permeable to water, so water leaves those tubular regions along with the sodium.
Activation of the renin-angiotensin-aldosterone system causes increased sodium retention by the kidneys, which leads to reduced water loss into the urine and therefore blood volume expansion. RAAS activation occurs during heart failure, which leads to fluid retention in the body. RAAS activation also occurs with renal artery stenosis, which is one cause of secondary hypertension. Drugs that block the formation of angiotensin II , or block aldosterone receptors enhance sodium and water loss, and thereby reduce blood volume. Therefore, any mechanism or drug that alters the activity of the renin-angiotensin-aldosterone system will affect blood volume.
You May Like: What Laxative Is Safe With Kidney Disease
Why Are The Kidneys So Important
Most people know that a major function of the kidneys is to remove waste products and excess fluid from the body. These waste products and excess fluid are removed through the urine. The production of urine involves highly complex steps of excretion and re-absorption. This process is necessary to maintain a stable balance of body chemicals.
The critical regulation of the body’s salt, potassium and acid content is performed by the kidneys. The kidneys also produce hormones that affect the function of other organs. For example, a hormone produced by the kidneys stimulates red blood cell production. Other hormones produced by the kidneys help regulate blood pressure and control calcium metabolism.
The kidneys are powerful chemical factories that perform the following functions:
- remove waste products from the body
- remove drugs from the body
- balance the body’s fluids
- release hormones that regulate blood pressure
- produce an active form of vitamin D that promotes strong, healthy bones
- control the production of red blood cells
Below you will find more information about the kidneys and the vital role they play in keeping your body functioning.
Sex Differences In Programmed Renal Hypertension
Sex differences in blood pressure regulation and in the progression of hypertension have been shown in both clinical and animal models. The renal RAAS functions in a sexually dimorphic manner to regulate renal function and the cardiovascular system. The different RAAS levels in the kidney of normal female and male rodents have been shown in many reports. When evaluating renal function and blood pressure of adult offspring exposed to intrauterine adverse environments, conditions of male offspring seem to be worse than those of females in most cases. The enhanced responsiveness to Ang II is testosterone-dependent in male IUGR offspring.96 As for females, the sensitivity to Ang II is modulated by ovarian hormones.97 Sex hormones differentially interact with RAAS pathways, with testosterone increasing expression of renin, AT1R, and upregulating vasopressor responses, while estrogen increases ACE2 and AT2R expression, which are considered beneficial for blood pressure.
Swasti Tiwari, Carolyn A. Ecelbarger, in, 2009
Recommended Reading: What Std Messes With Your Kidneys
Therefore The Kidneys Function In The Body:
Control blood composition and eliminate waste by filtration / reabsorption / secretion
Blood pressure affected by renin secretion.
Vitamin D helps regulate body calcium through activation.
If for some reason, the kidneys are not working, kidney dialysis methods become the only option to help the patient survive by cleaning the blood. This is especially necessary when both kidneys fail.
What Is The Role Of And In Regulation Of Kidney Function
The regulation of kidneys functioning is under the control of a complex hormonal mechanism regulated by the Antidiuretic hormone , Renin-Angiotensin-Aldosterone System and Atrial Natriuretic Factor . Kidney functions are also auto regulated as well as regulated by the neural system.Regulation by Antidiuretic hormone or Vasopressin: When osmolarity of blood increases, i.e., blood gets hypertonic above 300 mOsm/L, then osmoreceptors present in the brain get stimulated.1. Stimulation of these osmoreceptors cells, in turn, stimulate the hypothalamus, which leads to ADH secretion in the blood from the posterior pituitary lobe.2. ADH promotes the development of aquaporins in the Distal Convoluted Tubule and Collecting duct, and thus increases the reabsorption of water.3. Due to the reabsorption of water, the osmolarity of blood starts decreasing, and the urine becomes more concentrated.4. Also, in the hypothalamus, it stimulates thirst centres causing the sensation to drink water and reduce the hypertonicity of blood.5. The decrease in osmolarity of blood and increase in blood pressure results in an increase in GFR.
Don’t Miss: Pomegranate Juice Good For Kidney Stones
Systemic Arterial Pressure And Age
Fetal blood pressure
In pregnancy, it is the fetal heart and not the mother’s heart that builds up the fetal blood pressure to drive blood through the fetal circulation. The blood pressure in the fetal aorta is approximately 30 mmHg at 20 weeks of gestation, and increases to approximately 45 mmHg at 40 weeks of gestation.
The average blood pressure for full-term infants:
- Systolic 6595 mmHg
| 95140 | 6090 |
In children, the normal ranges for blood pressure are lower than for adults and depend on height. Reference blood pressure values have been developed for children in different countries, based on the distribution of blood pressure in children of these countries.
Aging adults
P2 Receptor Activation In Renal Tubular Segments
Sodium balance and regulation of ECFV is controlled by regulating sodium transport along the nephron. An increase in systemic blood pressure increases renal perfusion pressure to the kidney. While autoregulation is efficient, it is not perfect, leading to a subtle increase in glomerular capillary pressure and a small increase in glomerular filtration rate which can increase tubular fluid flow rate, stimulate ATP release from tubular epithelium where it can activate P2 receptors and reduce epithelial sodium transport. Therefore, regulation of ECFV occurs in part by P2-receptor-mediated regulation of salt and water reabsorption by the nephron .
Recommended Reading: Is Mulberry Good For Kidneys
Variable Or Fluctuating Blood Pressure
Some fluctuation or variation in blood pressure is normal. Variations in pressure that are significantly greater than the norm are associated with increased risk of cardiovascular disease brain small vessel disease, and dementia independent of the average blood pressure level. Recent evidence from clinical trials has also linked variation in blood pressure to stroke, heart failure, and cardiac changes that may give rise to heart failure. These data have prompted discussion of whether excessive variation in blood pressure should be treated, even among normotensive older adults. Older individuals and those who had received blood pressure medications are more likely to exhibit larger fluctuations in pressure, and there is some evidence that different antihypertensive agents have different effects on blood pressure variability whether these differences translate to benefits in outcome is uncertain.
High Blood Pressure And Kidney Failure
The kidneys nephrons are supplied with a dense network of blood vessels, and high volumes of blood flow through them. Over time, uncontrolled high blood pressure can cause arteries around the kidneys to narrow, weaken, or harden. These damaged arteries are not able to deliver enough blood to the kidney tissue.
Recommended Reading: Does Red Wine Cause Kidney Stones
Renal Basis For Essential Hypertension
Despite the complexity of blood pressure regulation, the central role of impaired renal sodium excretion in the genesis of hypertension is undisputed and continues to be supported by experimental and clinical studies. Subclinical renal abnormalities observed in some individuals with essential hypertension include focal renal ischemia leading to chronic non-suppressible renin secretion, renal sodium retention, reduced renal mass, decreased glomerular filtration rate, and a compromised sodium excretory capacity.49
Therapeutically, the role for renal sodium retention in the pathogenesis of hypertension is supported by the efficacy in many hypertensive individuals of diuretic therapy. Similarly, a role for non-suppressible renin secretion is supported by the efficacy of agents that interrupt the reninâangiotensin system.50 The relationship between subtle abnormalities in renal function and pregnancy outcome has not been investigated in detail. Given the significant impact of reduced renal function on the risk of preeclampsia, this is an area of investigation of potential importance.
Robert Fried Ph.D., in, 2014