Treatment Of Iron Deficiency Anemia In Ckd Nd
Iron supplementation can be administered either orally or intravenously . Oral iron is less expensive and easier to administer. However, i.v. iron enables the administration of larger doses of iron rapidly and is better tolerated . i.v. iron is superior to oral iron in achieving a sustained Hb response, reducing the need for blood transfusions and improving QOL in CKD .
The KDIGO, the National Kidney Foundation-Kidney Disease Outcomes Quality Initiative , and the anemia working group of the ERBP recommend iron supplementation in CKD with anemia and absolute or functional iron deficiency. While cut-off ferritin and TSAT levels for iron replacement initiation vary among these guidelines, there is general agreement on i.v. iron supplementation for CKD on dialysis and either i.v. or oral iron for CKD ND .
According to KDIGO guidelines, for adults with CKD and anemia who are not on iron or ESA therapy, a trial of i.v. iron is suggested . This is suggested if an increase in Hb concentration without starting ESA treatment is desired and TSAT is 30% and ferritin is 500 ng/mL . For adults with CKD on ESA who are not receiving iron supplementation, a trial of i.v. iron is recommended if an increase in Hb concentration is desired or a decrease in ESA dose is desired and TSAT is 30% and ferritin is 500 ng/mL .
The KDOQI commentary group reviewed these KDIGO recommendations and suggested that they may be too cautious regarding the use of i.v. iron .
Current Clinical Practice Guidelines Of Anemia In Ckd
Anemia management in CKD has evolved dramatically: from the first oral iron supplements introduced in 1830s , the use of red blood cell transfusions along the XX century, the appearance of the first rhuEPO use in late 1980s followed by long-acting ESAs, to finally, the widespread use of intravenous iron supplements in recent years. However, the actual management of anemia in patients with CKD varies among different countries and medical units . Indeed, current guidelines KDIGO ERBP NICE do not fully coincide with each other. Some controversies exist about the optimal Hb and iron targets. Table 1 summarizes the main differences.
Table 1. Summary of the key recommendations of the most recent anemia guidelines.
Further, these guidelines do not include more recent studies assessing the efficacy and safety of IV iron, as well as different strategies of iron repletion, which will probably change the clinical practice in the future. They demonstrate that in ND-CKD, renal transplant and PD patients IV iron is more efficacious and safe. In addition, a high-dose low frequency administration strategy in dialysis dependent chronic kidney disease patents is safe and improves outcomes in patients .
Hypoxia Inducible Factor System
EPO is a glycoprotein that binds to its receptor on the surface of erythroid progenitor cells mainly in the bone marrow, and serves as a key stimulus for red cell survival, proliferation and differentiation. EPO is produced predominantly by the fibroblast-like interstitial peritubular cells of the kidneys, and in a much lesser proportion, by the perisinusoidal cells in the liver, in response to changes in tissue oxygen tension . The production of EPO is controlled at the level of the EPO gene transcription. One of the most important factors that regulate its expression is the hypoxia-inducible factor system, whose activity depends on the tissue oxygen levels.
Under normoxic conditions, HIF1 is degraded. For this purpose, HIF1 is hydroxylated at two proline residues. This hydroxylation is performed by specific HIF prolyl-hydroxylase enzymes called prolyl hydroxylase domain enzymes that need the presence of oxygen, iron, and 2-oxoglutarate as co-factors. Three forms have been described: PHD1, PHD2, PHD3. PHD2 is the main isoform regulating HIF activity . Once HIF1 is hydroxylated, the E3 ubiquitin ligase von Hippel-Lindau binds HIF1, and is targeted for proteasomal degradation. In contrast, under low oxygen tension the action of PHDs is prevented, allowing for HIF1 stabilization and translocation to the nucleus . This pathway is the target of the new so-called hypoxia-inducible factor prolyl hydroxylase inhibitors .
Recommended Reading: Is Watermelon Bad For Kidneys
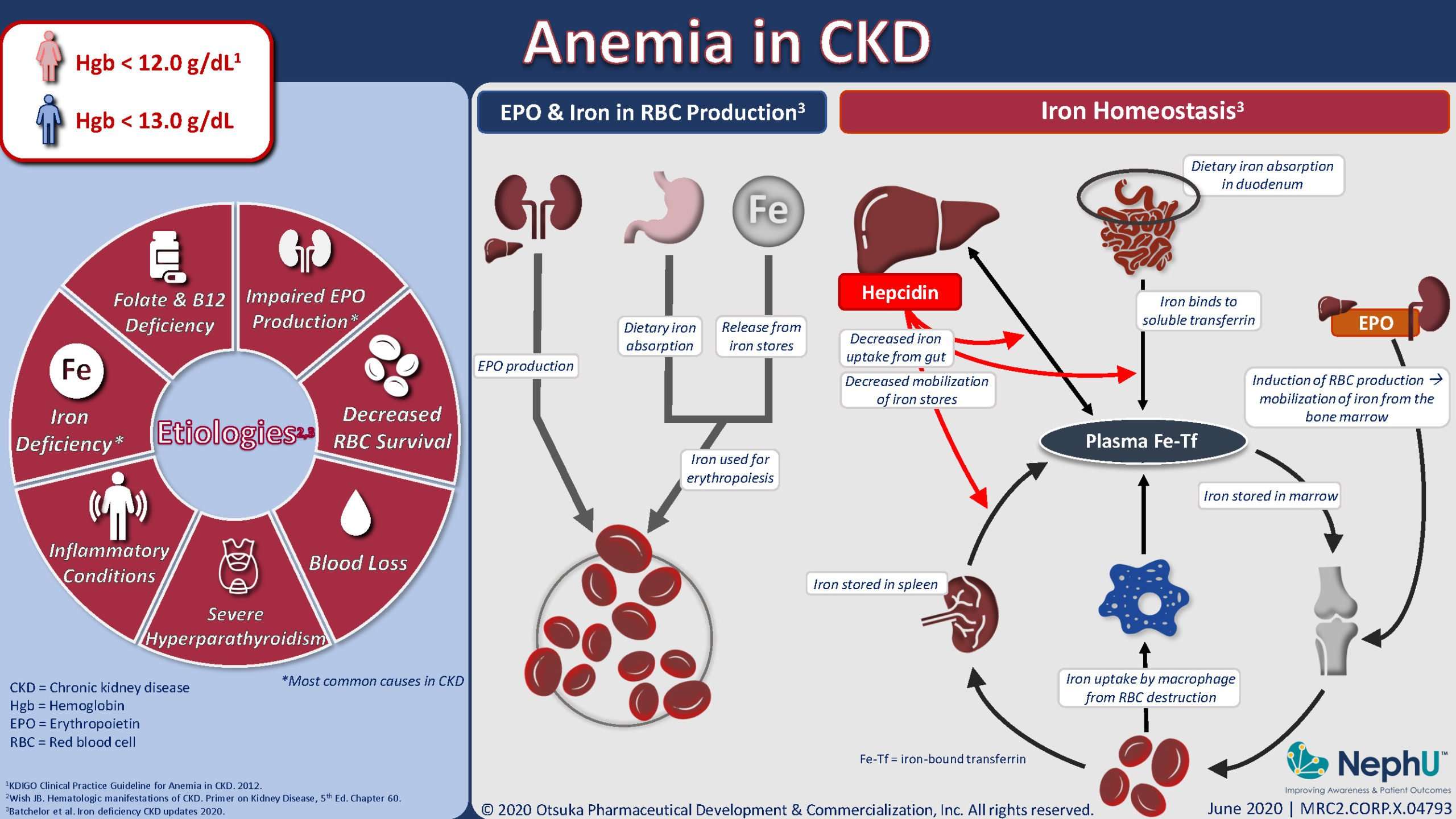
Anemia In Chronic Kidney Disease
If you have anemia, it means your blood is low on red blood cells or hemoglobin. Hemoglobin is a protein that red blood cells carry to help distribute oxygen throughout your body. In either case, it means that tissues and organs are not getting enough oxygen to function well without treatment.
Its estimated that people with kidney disease have anemia, according to the National Institutes of Health. Youre more likely to develop anemia as kidney disease advances.
Mild anemia doesnt always cause symptoms. But symptoms of anemia in CKD can include:
- fatigue
- malnutrition
- blood loss, including from frequent blood draws or dialysis treatment
With anemia, your body isnt making enough red blood cells. If you have anemia and CKD, your red blood cells may also have a shorter lifespan than usual. They can die off faster than your body can replace them.
Treatment for anemia will depend on why your body isnt making enough red blood cells or hemoglobin. Once the underlying cause is determined, treatment options may include the following:
Prolyl Hydroxylase Inhibitors: Oral Agents Activating The Hypoxia Inducible Factor
A better understanding of the response of the body to hypoxia and the related oxygen sensing system has clarified the central role of the hypoxia-inducible factors in EPO production. PHDi produce effects in the body that are similar to those occurring at high altitude exposure, inducing the bone marrow to produce more red blood cells. The HIF system not only upregulates EPO receptors, but also increases iron mobilization from the gut and macrophages through hepcidin-dependent and independent pathways . Hepcidin is usually upregulated in CKD and limits iron absorption and mobilization contributing to functional iron deficiency PHDi have been shown to significantly reduce hepcidin levels, likely through indirect mechanisms .
Also Check: Ibuprofen Processed By Liver Or Kidney
Management Of Anemia Of Ckd
The preferred initial therapy for anemia of chronic kidney disease is the use of erythropoiesis-stimulating agents . ESAs available in the United States include epoetin alfa and darbepoetin alfa .
The US Food and Drug Administration advises clinicians to consider starting ESA treatment for patients with CKD when the hemoglobin level is less than 10 g/dL, but does not define how far below 10 g/dL would be an appropriate threshold for initiating ESA treatment in an individual patient. Kidney Disease: Improving Global Outcomes guidelines suggest basing the decision whether to initiate ESA therapy in nonâdialysis-dependent CKD patients with a hemoglobin concentration < 10.0 g/dL on the following:
- Rate of fall of the hemoglobin concentration
- Prior response to iron therapy
- Risk of needing a transfusion
- Risks related to ESA therapy
- Presence of symptoms attributable to anemia
To evaluate response to ESA treatment, the KDIGO guidelines recommend measuring hemoglobin at least monthly during the initiation phase. During the maintenance phase, measurement is recommended at least every 3 months in patients with nonâdialysis-dependent CKD patients, and at least monthly in CKD 5D patients.
In 2011, the FDA abandoned the concept of a target range for the hemoglobin level in ESA treatment. Instead, the FDA recommended using the lowest dose of ESA sufficient to reduce the need for red blood cell transfusions for each patient, and adjusting the dose as appropriate.
How Does Chronic Kidney Disease Cause Anemia
Anybody can develop anemia, but it is very common in people with CKD. People with CKD may start to have anemia in the early stages of CKD, but it is most common in stages 3-5. Anemia usually gets worse as CKD gets worse. If your kidneys are not working as well as they should, you are more likely to get anemia.
If you think you might have CKD, talk to your doctor about getting tested. Management of anemia and its symptoms may help you feel better.
Also Check: Kidney Failure Kidney Disease Ribbon Tattoos
Definitions And Diagnosis Of Iron Deficiency In Ckd Patients
CKD may be associated with either absolute or functional iron deficiency. Functional iron deficiency may be related to the administration of erythropoiesis-stimulating agents which rapidly increases erythropoiesis. In this situation, total body iron stores are adequate, but iron release from stores into the circulation is not rapid enough to provide sufficient iron to support the increased erythropoietic rate driven by the ESA. In addition, in CKD, concomitant anemia of chronic disease is often present, which is related to an underlying inflammatory state and mediated partly by hepcidin, the levels of which were found to be increased in CKD .
It is difficult to determine whether functional iron deficiency is related to ESA or to anemia of chronic disease with an inflammatory block of available iron.
All CKD patients, particularly those with an estimated GFR < 60 mL/min/1.73 m2, should be screened for anemia on initial evaluation for CKD. Anemia is defined as Hb < 13 g/dL in men and Hb < 12 g/dL in women, according to WHO criteria . These thresholds are accepted by 2012 Kidney Disease: Improving Global Outcomes guidelines . The European Renal Best Practice position statement suggested adapting these thresholds to the European population . They suggest that a diagnosis of anemia should be made and further evaluation should be undertaken when Hb concentrations are < 13.5 g/dL in adult males and < 12.0 g/dL in adult females.
Impact Of Anaemia In Ckd Patients
-
Anaemia in CKD patients is associated with cardiovascular complications. Anaemia has been independently associated with the development of left ventricular hypertrophy . LVH, present in up to 74% of patients at the initiation of renal replacement therapy, is an independent predictor of subsequent cardiac morbidity and mortality .
-
The presence of anaemia early in end-stage renal disease is also associated with a greater rate of subsequent hospitalizations and mortality .
-
The effect of anaemia correction on the progression of CKD is controversial, with some studies showing a positive impact , and other studies showing no change in disease progression .
-
CKD patients suffering from anaemia have an impaired quality of life, exercise capacity, cognitive and sexual function .
-
Anaemia in CKD patients may increase blood transfusion requirements, and epoetin treatment decreases the number of transfusions .
Also Check: Is Ginger Good For The Kidneys
How Does Eating Diet And Nutrition Affect Anemia In Ckd
You may need to change what you eat to manage your anemia and CKD. Work with your health care professional or a registered dietitian to develop a meal plan that includes foods that you enjoy eating while maintaining your kidney health and managing your anemia.
If your body doesnt have enough iron, vitamin B12, or folate, your health care professional or a dietitian may suggest that you add more foods with these nutrients to your diet. However, some of these foods have high amounts of protein, sodium, or phosphorus, which people with CKD may need to limit. Talk with your health care professional or a dietitian before making any changes to your diet.
Erythropoietin Production Is Triggered By Hypoxia Mediated By Hif
Erythropoietin is produced primarily in the deep cortex and outer medulla of the kidneys by a special population of peritubular interstitial cells. The parenchymal cells of the liver also produce erythropoietin, but much less.
The rate of renal erythropoietin synthesis is determined by tissue oxygenation rather than by renal blood flow production increases as the hemoglobin concentration drops and the arterial oxygen tension decreases .
The gene for erythropoietin is located on chromosome 7 and is regulated by HIF. HIF molecules are composed of an alpha subunit, which is unstable at high Po2, and a beta subunit, constitutively present in the nucleus.
In hypoxic conditions, the HIF dimer is transcriptionally active and binds to specific DNA recognition sequences called hypoxia-response elements. Gene transcription is up-regulated, leading to increased production of erythropoietin.
Under normal oxygen tension, on the other hand, the proline residue of the HIF alpha subunit is hydroxylated. The hydroxylated HIF alpha subunit is then degraded by proteasomal ubiquitylation, which is mediated by the von Hippel-Lindau tumor-suppressor gene pVHL. Degradation of HIF alpha prevents formation of the HIF heterodimers. HIF therefore cannot bind to the hypoxia-response elements, and erythropoietin gene transcription does not occur.
Thus, in states of hypoxia, erythropoietin production is upregulated, whereas with normal oxygen tension, production is downregulated.
Recommended Reading: Watermelon Is Good For Kidney
Iron Metabolism Is Controlled By Several Proteins
Iron is characterized by its capacity to accept or donate electrons. This unique property makes it a crucial element in many biochemical reactions such as enzymatic activity, DNA synthesis, oxygen transport, and cell respiration.
Iron metabolism is under the control of several proteins that play different roles in its absorption, recycling, and loss .
Iron absorption and metabolism is controlled by several proteins.
DMT1 = divalent metal transporter 1 FPN = ferroportin Hgb = hemoglobin TF = transferrin, TFR = transferrin receptor
Dietary iron exists primarily in its poorly soluble trivalent ferric form , and it needs to be reduced to its soluble divalent ferrous form by ferric reductase to be absorbed. Ferrous iron is taken up at the apical side of enterocytes by a divalent metal transporter and is transported across the brush border.
To enter the circulation, iron has to be transported across the basolateral membrane by a transporter called ferroportin. Ferroportin is also found in placental syncitiotrophoblasts, where it transfers iron from mother to fetus, and in macrophages, where it allows recycling of iron scavenged from damaged cells back into the circulation. Upon its release, the ferrous iron is oxidized to the ferric form and loaded onto transferrin. This oxidation process involves hephaestin, a homologue of the ferroxidase ceruloplasmin.
Who Is More Likely To Have Anemia In Ckd
Your risk for anemia increases as your kidney disease gets worse.
People with CKD who also have diabetes are at greater risk for anemia, tend to develop anemia earlier, and often have more severe anemia than people with CKD who dont have diabetes.4 People older than 60 are also more likely to have anemia with CKD.5
Read Also: Acv And Kidneys
When Does Anaemia Begin
Anaemia may begin to develop in the early stages of kidney disease for example in CKD Stage 2 when you still have 6090% of normal kidney function. The blood creatinine level may only be marginally raised at this point, at 120150 mcmol/L for example . Anaemia worsens as kidney disease progresses. End-stage kidney disease , the point at which dialysis or a kidney transplant becomes necessary, doesnt occur until you have only about 10% of your kidney function remaining. Nearly everyone with end-stage kidney disease has anaemia, and will need treatment.
How Is Anemia Related To Chronic Kidney Disease
Anemia is a common complication of chronic kidney disease . CKD means your kidneys are damaged and cant filter blood the way they should. This damage can cause wastes and fluid to build up in your body. CKD can also cause other health problems.
Anemia is less common in early kidney disease, and it often gets worse as kidney disease progresses and more kidney function is lost.
You May Like: Wine And Kidney Stones
Effects Of Esa Therapy At A Cellular Level
Early data showed that ESA increases vascular resistance and resistance to the vasodilatory action of nitric oxide via impact on calcium influx in vascular smooth muscle cells. ESA also has autocrine or paracrine actions, for example on the brain . It increases the number of circulating erythrocytes primarily by preventing apoptosis of erythroid progenitors. In vitro , ESA prevents neuronal apoptosis. Results of recent studies show that systemically administered ESA is neuroprotective in vivo .
ESA stimulates angiogenesis
The number of circulating stem cells increased with low doses of ESA treatment in haemodialysis patients. Endothelial progenitor cell proliferation and differentiation is also regulated by ESA .
In vivo pleiotropic renoprotective actions of ESA
Several in vivo investigations have shown that ESA can reduce the renal dysfunction and injury caused by oxidative stress, hypoxia and haemorrhagic shock, generally by reducing caspase activation and apoptotic cell death .
Clinical trials will be needed to confirm these renoprotective effects in man. However a phase II trial with ESA in patients with acute ischaemic stroke yielded promising results .
Treatment For Kidney Disease Anemia
For Chronic Kidney Disease Dialysis At this stage, your kidneys can no longer eliminate waste as fast as you’re producing it. There are two treatment options for end-state kidney disease:
ESA therapy. ESAs and iron are the mainstays of treatment for anemia associated with CKD. ESAs are used to stimulate erythropoiesis by either directly or.
Before starting anemia treatment, your doctor will order tests to find the exact cause of your anemia. why do people with kidney disease get anemia? Your kidneys make an important hormone called erythropoietin . Hormones are secretions that your body makes to help your body work and keep you healthy. EPO tells your body to make red blood.
If a patient’s hemoglobin does not go up after beginning treatment with an erythropoiesis-stimulating agent, the doctor will recheck iron. Even though there is now a.
What is anemia of chronic kidney disease? Anemia means that you do not have enough red blood cells. Red blood cells carry oxygen from your lungs to your.
For individuals with CKD it is important to treat anemia because there are many risks to having low hemoglobin levels. Treating anemia can.
Why do people with kidney disease get anemia? Your kidneys.
treat anemia? Your treatment will depend on the exact cause of your anemia.
Chinese Medicine Chronic Kidney Disease With unproper treatment, stage 3 chronic kidney disease will progress into stage 4, at which stage the kidney function will be severely decreased. So it
May 20, 2020.
Don’t Miss: Carbonation And Kidney Stones