Role Of Apical Membrane Na+
Molecular characteristics of NHEs in proximal tubules
Localization and redistribution of NHE3 during acute hypertension. The endocytic compartment of the proximal tubule was labeled by intravenous injection of horseradish peroxidase , and rats were sham operated , or blood pressure was increased for 20 min . Kidneys were fixed in situ, sectioned, and double labeled with either polyclonal anti-NHE3 or monoclonal anti-HRP . NHE3 is retracted from the body to the base of the microvilli during acute hypertension, with no evidence that NHE3 moves into endocytic tracer HRP-labeled compartment. Reproduced from McDonough with permission .
Expression and localization of NHEs in proximal tubules
Role Of Intraluminal Factors
Flow-dependent fluid reabsorption
Flow-dependent fluid reabsorption in proximal tubules remains a well-recognized phenomenon today. Wiederholt et al. first showed that absolute proximal reabsorption changed in direct proportion to tubular flow or perfusion rate. These authors observed a constancy of proximal tubular fluid to plasma inulin concentration ratio, under conditions in which proximal tubular flow rate was altered without changes in single nephron GFR or peritubular physical factors . This phenomenon was later confirmed by many others , providing evidence of flow-dependent of proximal tubular fluid reabsorption.
However, the nature of glomerular-borne factors still remains to be determined. One of possible glomerular-borne factors may be HCO3â. Mathisen and coworkers used ethacrynic acid to inhibit proximal tubular carbonic anhydrase and reported a direct proportionality between HCO3â and absolute proximal fluid reabsorption . Green et al. perfused proximal tubular lumen with HCO3â-Ringer solution and obtained 80% effective GTB . Other potential glomerular-borne factors may include organic solutes such as glucose, lactate, alanine, or citrate. Removal of these organic solutes from proximal tubular perfusates impaired GTB by almost 45â75%, whereas addition of these solutes in the perfusates increased absolute proximal reabsorption . These studies suggest that glomerular-borne factors may at least account for up to one-third of a perfect GTB.
Early Forms Of The Kidney
The common representation of mammalian kidney development includes three successive phases beginning with the appearance of the pronephros, the developmental homologue of the type of kidney found in only the lowest vertebrates. In human embryos, the first evidence of a urinary system consists of the appearance of a few segmentally arranged sets of epithelial cords that differentiate from the anterior intermediate mesoderm at about 22 days’ gestation. These structures are more appropriately called nephrotomes. The nephrotomes connect laterally with a pair of primary nephric ducts, which grow toward the cloaca . The earliest stages in the development of the urinary system depend on the action of retinoic acid, which sets the expression limits of Hox 4-11 genes that determine the craniocaudal limits of the early urinary system. The molecular response by the intermediate mesoderm is the expression of the transcription factors Pax-2 and Pax-8, which then induce Lim-1 in the intermediate mesoderm. Lim-1 is required for the aggregation of the mesenchymal cells of the intermediate mesoderm into the primary nephric ducts.
Early in the 5th week of gestation, the ureteric bud begins to grow into the most posterior region of the intermediate mesoderm. It then sets up a series of continuous inductive interactions leading to the formation of the definitive kidney, the metanephros.
Figure 2. Stages in the formation of the metanephros. At 6 weeks. At 7 weeks. At 8 weeks. At 3 months .
Read Also: How Long After Kidneys Shut Down Until Death
Where Does The Kidney Filter The Blood
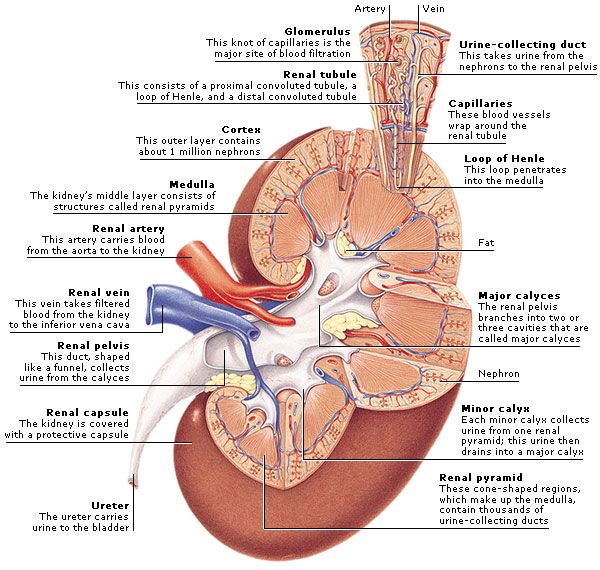
Blood flows into your kidney through the renal artery. This large blood vessel branches into smaller and smaller blood vessels until the blood reaches the nephrons. In the nephron, your blood is filtered by the tiny blood vessels of the glomeruli and then flows out of your kidney through the renal vein.
Role Of Basolateral Membrane Na+/ca2+ Exchanger In Sodium Transport
Molecular characteristics of Na+/Ca2+ exchanger
The molecular and protein structures and physiological implications of the sodium and calcium exchanger in the kidney and other physiological systems have been reviewed elsewhere . This section only reviews the role of basolateral membrane Na+/Ca2+ exchanger in sodium transport in proximal tubules. The Na+/Ca2+ exchanger gene was first cloned from the dog and human cardiac muscle . The super family of the Na+/Ca2+ exchangers consists of three gene members, NCX1, NCX2 and NCX3 . The NCX gene family is widely expressed in different mammalian tissues . While the localization and functional significance of the Na+/Ca2+ exchanger have been extensively studied in cardiac tissues and vascular smooth muscle cells , its role in the regulation of sodium transport in proximal tubules remains poorly understood. In the kidney, localization of the Na+/Ca2+ exchanger in the basolateral membranes of proximal tubules remains an issue of debate .
Effects of Na+/Ca2+ exchanger on sodium transport in proximal tubules
Mechanisms underlying Na+/Ca2+ exchanger-regulated sodium transport in proximal tubules
You May Like: Can Exercise Help Pass Kidney Stones
Proximal Tubular Functions And Glomerulo
Over the last two decades, gene silencing or deletion has been increasingly used to generate unique animal models in which a gene encoding a particular enzyme, protein, GPCR, or transporter is silenced or deleted globally throughout the body or in a cell- or tissue-specific manner. These novel animal models has provided a powerful tool to further study the proximal tubular function and determine the genetic and signaling mechanisms by which the proximal tubular function is regulated. However, some interesting but unexpected findings and/or insights on the proximal tubular function and GTB have emerged during recent years. Several examples are briefly reviewed below.
What Keeps The Kidneys In Place
Each kidney is held in place by connective tissue, called renal fascia, and is surrounded by a thick layer of adipose tissue, called perirenal fat, which helps to protect it. A tough, fibrous, connective tissue renal capsule closely envelopes each kidney and provides support for the soft tissue that is inside.
Also Check: Are Probiotics Bad For Kidneys
What Are The Three Main Regions Of The Kidney
The kidney is made up of three different regions internally: the outer cortex the middle medulla and the inner-most renal pelvis.The kidney is made up of three different regions internally: the outer cortex the middle medulla and the inner-most renal pelvis
the funnel-like dilated part of the ureter in the kidney
Regulation Of Nhe3 Activity In Proximal Tubules
Effects of 2 week infusion of the non-pressor dose of ANG II and concurrent losartan treatment on phosphorylated NHE3 immunofluorescence staining or phospho-NHE3 protein abundance in membrane fractions of proximal tubules of the rat kidney . 100 µg proteins were loaded in each lane.of western blot gels. *p< 0.05 or **p< 0.01 vs. control â â p< 0.01 vs. ANG II-infused rats. Reproduced from Li and Zhuo .
New insights and perspectives into the roles of NHE3 in the regulation of proximal tubule sodium transport and blood pressure, as revealed from studies on NHE3 transgenic mice
Effects of global NHE3 gene knockout on proximal tubule fluid and bicarbonate absorption and blood pressure in adult Slc9a3+/+ and Slc9a3â/â mice. a,b, In situ microperfusion of proximal convoluted tubules revealed that fluid and HCO3â absorption were sharply reduced in Slc9a3â/â tubules relative to Slc9a3+/+ tubules . ** P< 0.001 Jv, fluid absorption JHCO3, HCO3â absorption. c, Blood-pressure measurements using the tail-cuff method showed that systolic pressure was significantly reduced in awake Slc9a3â/â mice . d, Blood-pressure measurements using a femoral artery catheter showed that mean arterial pressure was reduced in anaesthetized Slc9a3â/â mice compared with both Slc9a3+/â and Slc9a3+/+ mice. Values for all analyses are mean s.e.m. Reproduced from Schultheis et al. .
Also Check: What Does A Human Kidney Look Like
What Are Kidney Failure And End
Kidney failure is the acute or chronic loss of 85 percent or more kidney function. End-stage renal disease , is kidney failure that is treated by dialysis or kidney transplant. Depending on the form of glomerular disease, kidney function may be lost in a matter of days or weeks or may deteriorate slowly and gradually over the course of decades.
What Are The First Signs Of Kidney Problems
Signs of Kidney Disease
- You’re more tired, have less energy or are having trouble concentrating. …
- You’re having trouble sleeping. …
- You have dry and itchy skin. …
- You feel the need to urinate more often. …
- You see blood in your urine. …
- Your urine is foamy. …
- You’re experiencing persistent puffiness around your eyes.
Read Also: Can Breast Cancer Spread To Your Kidneys
What Are The First Signs Of A Kidney Problem
Kidney Disease Signs Youre more tired, less energetic, or having trouble concentrating. Youre having trouble sleeping.
You have itchy and dry skin. You feel compelled to urinate more frequently. Blood can be found in your urine.
Your urine is foamy. Youre having trouble puffing around your eyes on a regular basis.
How Is Glomerular Disease Diagnosed
Patients with glomerular disease have significant amounts of protein in the urine, which may be referred to as “nephrotic range” if levels are very high. Red blood cells in the urine are a frequent finding as well, particularly in some forms of glomerular disease. Urinalysis provides information about kidney damage by indicating levels of protein and red blood cells in the urine. Blood tests measure the levels of waste products such as creatinine and urea nitrogen to determine whether the filtering capacity of the kidneys is impaired. If these lab tests indicate kidney damage, the doctor may recommend ultrasound or an x-ray to see whether the shape or size of the kidneys is abnormal. These tests are called renal imaging. But since glomerular disease causes problems at the cellular level, the doctor will probably also recommend a kidney biopsyâa procedure in which a needle is used to extract small pieces of tissue for examination with different types of microscopes, each of which shows a different aspect of the tissue. A biopsy may be helpful in confirming glomerular disease and identifying the cause.
You May Like: How Do You Spell Kidney
Kidney Function And Risk Factors
The preoperative clinical evaluations of patients with renal tumor were reviewed to obtain height, body mass index , serum creatinine , 24-hour urine protein, hypertension status , and diabetes mellitus . The GFR was estimated using the creatinine-based CKD Epidemiology Collaboration equation. The 24-hour urine protein excretion was estimated from a spot urine protein-to-osmolality ratio. Three orthogonal linear dimensions on the preoperative computed tomography or magnetic resonance imaging scan were used to estimate renal tumor volume .
Role Of Basolateral Membrane Na+
It was well established in the 1960s to 1970s that in proximal tubules, sodium is primarily reabsorbed via an active transport process mediated by an energy-dependent mechanism . Wesson and Anslow appeared to first suggest that sodium might be actively transported across the proximal tubular epithelium against a sodium concentration gradient, but had no direct evidence to support the hypothesis at the time . Kokko et al. subsequently showed that the sodium concentration gradient was developed apparently due to fluid retention within the tubular lumen by the nonelectrolytes, while sodium transport continuously proceeded . In addition to the sodium concentration gradient, sodium transport appears to occur against a transtubular electrical potential gradient as well, with the proximal tubular lumen being about 20 mv negative vs. the interstitial and peritubular fluid . However, later studies found that the transtubular electrical gradient across proximal convoluted tubules was probably smaller than previously reported, which only ranged from â6 to +2 mv . Nevertheless, it is still possible that even such smaller transepithelial electrical gradient may play an important role in the regulation of proximal tubular sodium transport.
Molecular characteristics of Na+-K+-ATPase
Expression and localization of Na+-K+-ATPase in proximal tubules of the nephron
Effects of Na+-K+-ATPase on sodium transport in proximal tubules
Also Check: What Do The Kidneys Do For Your Body
Characteristics Of Patients With Renal Tumor
We identified and obtained kidney wedge sections of 845 patients with a renal tumor. Ten patients were excluded for specific renal diseases on pathology: one each for amyloidosis, ESRD histology, severe chronic lymphocytic pyelonephritis, chronic interstitial nephritis, lymphomatous interstitial nephritis, crescentic GN, severe nodular glomerulosclerosis, FSGS with collapsing features, IgA nephropathy, and diffuse mesangial sclerosis with FSGS. Another 23 patients were excluded for missing clinical characteristics resulting in a sample size of 812 patients. Diabetic nephropathy occurred with mild to moderate diffuse mesangial expansion in 28 patients and nodular sclerosis in 12 patients these were all included in glomerular volume and %GSG estimates. Segmental sclerosis occurred in 29 patients but was minimal when present these were included in glomerular volume estimates. The demographic, clinical, and overall pathologic characteristics of the cohort are presented in . The median tumor volume was 100 cm3 . The number of patients and numbers of nonsclerotic and globally sclerotic glomerular profiles in each of three cortical regions, per each decade of life, is presented in Supplemental Table 1.
Unadjusted associations of %GSG category in three cortical regions with other biopsy pathology
Isotonic Fluid Absorption In Proximal Tubules
Historical considerations
The mechanisms underlying isosmotic fluid reabsorption may involve several hypotheses. As in other leaky epithelia such as small intestines and gall bladder, it was widely thought early that fluid transport by proximal tubular epithelium is a passive process as a result of active sodium and solute reabsorption. This is because active sodium and solute transport across proximal tubular epithelium creates an effective transepithelial osmotic gradient that drives water down an osmotic gradient. However, this explanation may be too simplistic, given the complexity of sodium and fluid reabsorption in proximal tubules of the kidney especially in vivo. Over the last 50 years, several hypotheses have been put forwarded to explain isosmotic fluid reabsorption in proximal tubules of the kidney, as discussed below.
Role of lateral intercellular space hypertonicity
Role of Na+ recirculation
Role of intraluminal hypotonicity
Role of axial anion asymmetry
Role of Aquaporin 1
Osmolality in plasma and late proximal tubular fluid in aquaporin-1 -knockout and wild-type mice. Values are means ±SE and are shown for AQP1 +/+ , AQP1 â/â , and hydrated AQP1 â/â mice . A: relationship between absolute values of osmolalities in plasma and late proximal tubule fluid . B: transtubular osmotic gradients, i.e., the osmolality differences between plasma and LPT. * P< 0.001 compared with AQP1 +/+ mice. Reproduced from Vallon et al. with permission .
Recommended Reading: Is Creatine Bad For Your Kidneys
Emt/met In Regenerating Kidney Tubule Epithelium
Nephrons of the mammalian kidney do not regenerate after their destruction, but kidney tubule epithelium regenerates after injury. The epithelial cells have a low basal rate of maintenance regeneration, as evaluated by PCNA and Ki-67 staining for mitosis . A standard injury model to demonstrate injury-induced regeneration of tubule epithelium is ischemia followed by reperfusion, in which the blood supply to the kidney is temporarily clamped off and the kidney then allowed to reperfuse. Under these circumstances, epithelial cells die and are sloughed off their basement membrane, but are rapidly replaced .
Tubule epithelial cells undergo EMT to form proliferating mesenchymal cells that migrate to cover the denuded areas of the basement membrane . The mesenchymal cells express vimentin and -smooth muscle actin, as well as Pax-2, a transcription factor critical for kidney ontogenesis . In preparation for migration, integrins are relocated from basal to lateral borders, NCAM expression is increased, and Fn, HA, uPA, and MMP-2 and 9 are upregulated . Another molecule involved in mesenchymal migration is kidney injury molecule-1 , a transmembrane protein of the Ig superfamily that is strongly upregulated in the post-ischemic rat kidney . After re-covering the denuded areas of the basement membrane, the mesenchymal cells undergo MET to restore the epithelium.
FIGURE 15.5. Kidney tubule epithelium regenerates by EMT/MET.
Bruce M. Carlson, in, 2015
What Are The Kidneys Seven Functions
A controlling ACID-base balance is one of the seven functions of the kidneys. W is the key to maintaining a healthy WATER balance.
E keeping your ELECTROLYTE balance in check. T Eliminating TOXINS and other waste products from the body. B is responsible for controlling BLOOD PRESSURE.
E the hormone ERYTHROPOIETIN is produced by E. Vitamin D is activated by vitamin D.
Don’t Miss: Can Kidney Stones Cause Fever
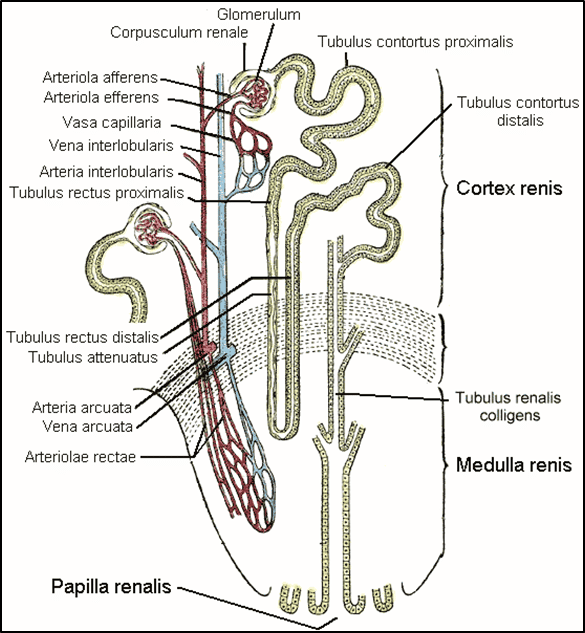
Superficial Vs Juxtamedullary Nephrons
The ultrastructure of proximal tubular segments in rodents and humans has been extensively studied and characterized . Proximal tubules of the nephron in animals and humans include proximal convoluted tubules, which are situated in the cortical labyrinth and connected directly to the glomerulus, via the Bowmanâs space, and proximal straight tubules in the inner cortex and outer stripe of the outer medulla . Only those proximal convoluted tubules of superficial nephrons usually traverse the cortical surface of the kidney, which are accessible to in vivo micropuncture or microperfusion investigations. By contrast, proximal convoluted tubules in juxtamedullary nephrons run deep into the medullary rays and are not accessible to micropuncture and microperfusion in vivo. Proximal convoluted tubules are approximately 25% longer in juxtamedullar nephrons than superficial nephrons . In vitro juxtamedullary preparation has been extensively used to study hemodynamic and vascular responses in juxtamedullar nephrons , but whether the preparation can be adapted for micropuncture or microperfusion of proximal tubules of juxtamedullary nephrons still remains uncertain. Accordingly, the current understanding of proximal tubular function, which is largely based on in vivo micropuncture studies, may only apply to the proximal convoluted tubules of superficial nephrons.
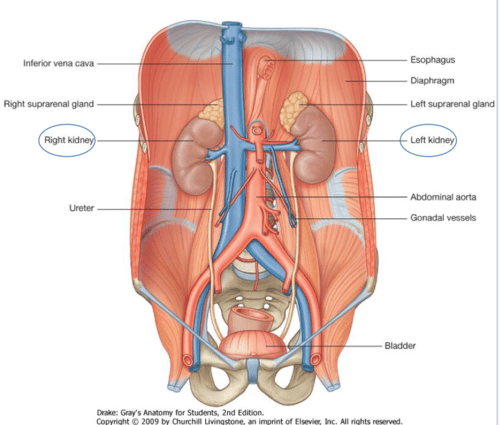
Clinical Relevance: Variation In Arterial Supply To The Kidney
The kidneys present a great variety in arterial supply these variations may be explained by the ascending course of the kidney in the retroperitoneal space, from the original embryological site of formation to the final destination . During this course, the kidneys are supplied by consecutive branches of the iliac vessels and the aorta.
Usually the lower branches become atrophic and vanish while new, higher ones supply the kidney during its ascent. Accessory arteries are common . An accessory artery is any supernumerary artery that reaches the kidney. If a supernumerary artery does not enter the kidney through the hilum, it is called aberrant.
Read Also: What Does It Mean When My Kidneys Ache