Treatment Of Anemia Of Renal Disease
-
Treatment of underlying renal disease
-
Sometimes, recombinant erythropoietin and iron supplements
Treatment of anemia of renal disease is directed at
-
Improving renal function
-
Increasing RBC production
If renal function returns to normal, anemia is slowly corrected.
In patients receiving long-term dialysis, recombinant erythropoietin, beginning with 50 to 100 units/kg IV or subcutaneously 3 times a week with iron supplements, is the treatment of choice. In almost all cases, maximum increases in RBCs are reached by 8 to 12 weeks. Reduced doses of EPO can then be given 1 to 3 times a week. Transfusions are rarely necessary. Careful monitoring of the response is needed to avoid adverse effects when hemoglobin increases to > 12 g/dL .
Evaluating And Diagnosing Anaemia In Ckd
Guideline 1.1 Evaluation of anaemia – screening for anaemia
We suggest that haemoglobin levels should be routinely measured to screen for anaemia:
-
at least annually in patients with CKD G3 and
-
at least twice a year in patients with CKD G45 not on dialysis
Guideline 1.2 – evaluation of anaemia Haemoglobin levels
We recommend that all patients with chronic anaemia associated with chronic kidney disease should be investigated for the cause and possible treatment, irrespective of the grade of kidney disease or requirement for renal replacement therapy if:
-
their haemoglobin levels are less than 110 g/L or
-
they develop symptoms attributable to anaemia
This is to ensure the correct diagnosis and management of anaemia.
Guideline 1.3 – evaluation of anaemia – renal function
We suggest that CKD should be considered as a possible cause of anaemia when the glomerular filtration rate is < 60 ml/min/1.73m2. It is more likely to be the cause if the GFR is < 30 ml/min/1.73m2 and no other cause, e.g. blood loss, folic acid or vitamin B12 deficiency, is identified.
Guideline 1.4 – evaluation of anaemia – erythropoietin measurement
We recommend that measurement of erythropoietin levels should not routinely be considered for the diagnosis or management of anaemia for patients with CKD.
Guideline 1.5 – Evaluation of anaemia Baseline investigations
We recommend that laboratory evaluation should include the following tests :
Full blood count includingin addition to the Hb concentration:
Iron Targets: How Much Iron Is Too Much Iron
Iron overload is a condition of elevated body iron content associated with signs of organ dysfunction that is presumably caused by excess iron. Some studies have demonstrated an increase in the liver iron content in hemodialysis patients, and an association between hepatic iron overload and hepatic steatosis has been recently described . However, its clinical relevance is still not known, and no deposits have been observed in other territories, such as cardiac or pancreatic . A metaanalysis of clinical trials and observational studies in the setting of hemodialysis suggests that patients that received higher doses of IV iron did not show a higher risk of mortality, infections or cardiovascular events . Nonetheless, the strength of the findings is limited by the small number of patients and of events in the clinical trials, and by the statistical heterogeneity in the observational studies included.
There has long been a concern whether iron supplements increased the risk of infections. A sub-analysis of PIVOTAL study did not show differences in infection episodes, hospitalization or death for infection between the proactive high dose regimen and reactive low dose-iron groups of patients .
Don’t Miss: Can High Bp Cause Kidney Damage
Management Of Anemia Of Ckd
The preferred initial therapy for anemia of chronic kidney disease is the use of erythropoiesis-stimulating agents . ESAs available in the United States include epoetin alfa and darbepoetin alfa .
The US Food and Drug Administration advises clinicians to consider starting ESA treatment for patients with CKD when the hemoglobin level is less than 10 g/dL, but does not define how far below 10 g/dL would be an appropriate threshold for initiating ESA treatment in an individual patient. Kidney Disease: Improving Global Outcomes guidelines suggest basing the decision whether to initiate ESA therapy in nonâdialysis-dependent CKD patients with a hemoglobin concentration < 10.0 g/dL on the following:
- Rate of fall of the hemoglobin concentration
- Prior response to iron therapy
- Risk of needing a transfusion
- Risks related to ESA therapy
- Presence of symptoms attributable to anemia
To evaluate response to ESA treatment, the KDIGO guidelines recommend measuring hemoglobin at least monthly during the initiation phase. During the maintenance phase, measurement is recommended at least every 3 months in patients with nonâdialysis-dependent CKD patients, and at least monthly in CKD 5D patients.
In 2011, the FDA abandoned the concept of a target range for the hemoglobin level in ESA treatment. Instead, the FDA recommended using the lowest dose of ESA sufficient to reduce the need for red blood cell transfusions for each patient, and adjusting the dose as appropriate.
Safety Of Hif Prolyl Hydroxylase Inhibitors
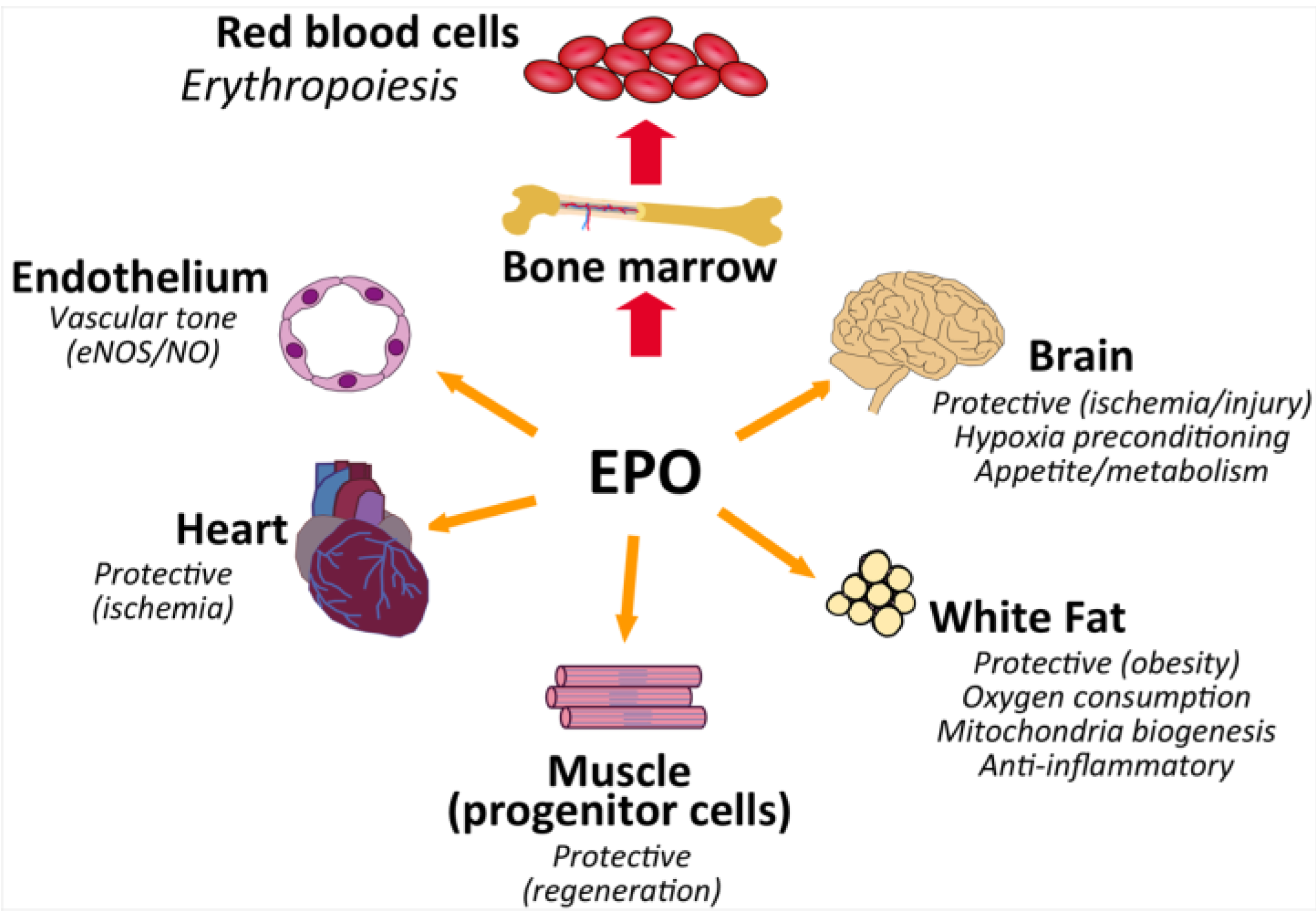
From a mechanistic point of view, the inhibition of prolyl-hydroxylases prevents HIF from degradation, leading to an increase of endogenous EPO within the physiological range, rather than the pharmacological levels achieved by current ESAs. Therefore, the rate of adverse events related to the high EPO levels should be expected to be lower than with ESAs. However, as mentioned before, HIF also modulates many other non-erythropoietic genes. This activity would explain the potential beneficial effects seen in pre-clinical and early clinical studies such as an improved iron utilization, HDL and LDL lowering effect, ischemia protection and a protective effect on CKD progression, improved neo-vascularization or better blood pressure control .
Nonetheless, potential deleterious side effects due to the modulation of other genes with this new class of drugs have also been postulated, notably tumor progression, enhanced vascular calcification, enhanced growth of renal cysts, worsening of retinopathy, or an increase in pulmonary artery pressure. In addition, whether these prolyl-hydroxylase inhibitors inhibit other di-oxygenases beyond HIF-PHIs and thus other pathways is unknown. Data from large phase III studies are still to be published and will surely help to answer these open questions.
Recommended Reading: Does Zofran Affect Kidney Function
Study Definitions And Design
The analysis was restricted to men contributing data after January 1, 1996 during the effective therapy era. We further limited the analysis to men with two consecutive hemoglobin measurements greater than 13 gm/dl at study entry to avoid prevalence bias and temporal ambiguities in the relationship between HIV infection and low hemoglobin levels. For men who were HIV infected, only AIDS-free time contributed to the analysis to exclude hemoglobin effects resulting from the occurrence of opportunistic infections and their treatment. The end of the analysis period was March 31, 2009.
Glomerular filtration rate was estimated at each 6-month visit using a serum creatinine-based estimating equation, the CKD-EPI equation. To assess the effect of impaired kidney function on hemoglobin levels, eGFR was dichotomized using a threshold of 60ml/min/1.73m2 following the National Kidney Foundation Kidney Disease Outcomes Quality Initiative guidelines for defining moderate to severe CKD.
What Is The Treatment Of Anemia Caused By Ckd
- Erythropoiesis Stimulating Agents These are drugs that will stimulate the production of RBCs in your bone marrow . Their main advantage is the reduced requirement of blood transfusions which can leave a patient in an iron overloaded state.
- Iron This is required by the bone marrow to make RBCs in your body. Without Iron all RBC production will cease even if you are given ESAs.
- Red Blood Cell Transfusion These are usually not required unless the hemoglobin count falls dangerously low.
- Vitamin B12 or Folic Acid Supplements Both these vitamins are required in the process of creating RBCs in your body. These may be prescribed to restore adequate amounts of these vitamins.
- Triferic This newly FDA approved drug is reportedly removing the need for post dialysis Iron therapy. The solution contains a dissolved form of Iron that is administered to a patient via a dialysis machine.
Disclaimer: The UCLA Health System cannot guarantee the accuracy of such information. The information is provided without warranty or guarantee of any kind. Please speak to your Physician before making any changes.
You May Like: What Causes Kidney Stone Pain
Anemia Management Esas And Covid 19
Regarding iron supplementation, systemic inflammatory processes as happens with severe COVID 19 decrease the availability of iron. Furthermore, iron is also essential for viral replication . In addition, patients with viral infections and iron overload have a poor prognosis. Therefore, limiting iron supplements could be beneficial for patients with severe COVID 19 although more studies are need to shed light into this subject .
Treatment Of Iron Deficiency Anemia In Ckd Nd
Iron supplementation can be administered either orally or intravenously . Oral iron is less expensive and easier to administer. However, i.v. iron enables the administration of larger doses of iron rapidly and is better tolerated . i.v. iron is superior to oral iron in achieving a sustained Hb response, reducing the need for blood transfusions and improving QOL in CKD .
The KDIGO, the National Kidney Foundation-Kidney Disease Outcomes Quality Initiative , and the anemia working group of the ERBP recommend iron supplementation in CKD with anemia and absolute or functional iron deficiency. While cut-off ferritin and TSAT levels for iron replacement initiation vary among these guidelines, there is general agreement on i.v. iron supplementation for CKD on dialysis and either i.v. or oral iron for CKD ND .
According to KDIGO guidelines, for adults with CKD and anemia who are not on iron or ESA therapy, a trial of i.v. iron is suggested . This is suggested if an increase in Hb concentration without starting ESA treatment is desired and TSAT is 30% and ferritin is 500 ng/mL . For adults with CKD on ESA who are not receiving iron supplementation, a trial of i.v. iron is recommended if an increase in Hb concentration is desired or a decrease in ESA dose is desired and TSAT is 30% and ferritin is 500 ng/mL .
The KDOQI commentary group reviewed these KDIGO recommendations and suggested that they may be too cautious regarding the use of i.v. iron .
Recommended Reading: Can Antibiotics Cause Kidney Failure
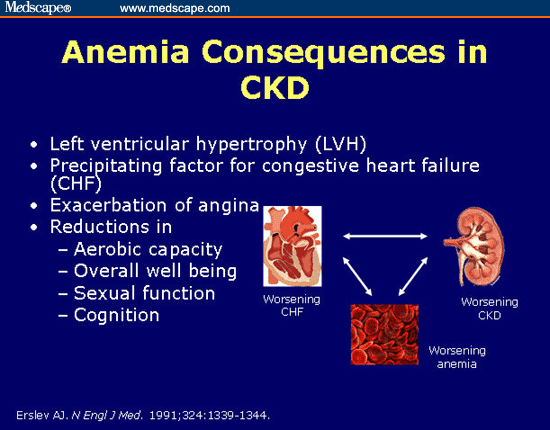
Renal Anemia Is Associated With Bad Outcomes
Anemia in chronic kidney disease is independently associated with risk of death. It is also an all-cause mortality multiplier, i.e., it magnifies the risk of death from other disease states.
In observational studies, anemia was associated with faster progression of left ventricular hypertrophy, inflammation, and increased myocardial and peripheral oxygen demand, thereby leading to worse cardiac outcomes with increased risk of myocardial infarction, coronary revascularization, and readmission for heart failure. Anemia is also associated with fatigue, depression, reduced exercise tolerance, stroke, and increased risk of rehospitalization.
Iron Supplementation For Anemia In Ckd
Guidelines acknowledge that the optimal strategy to manage iron metabolism remains unclear, and advocate for balancing the potential benefits and risks of iron supplementation . Table 1 summarizes the principles and targets of the management of iron supplements of the KDIGO ERBP NICE guidelines. In recent years some good quality pre-clinical studies, clinical trials and epidemiological studies have shed some light on the therapeutic approach regarding iron deficiency in CKD and will surely change clinical practice.
Intravenous iron has shown benefits both in DD-CKD and more recently in NDD-CKD, as it has proved to be more efficacious in rising ferritin and Hb levels, while reducing ESA and transfusion requirements. Specifically, in hemodialysis patients, oral preparations seem to be useless, maybe except for the phosphate binder ferric citrate . In addition, gastrointestinal intolerance and constipation reduce tolerance and compliance of oral iron formulations .
However, some concerns raised about IV iron formulation such as enhanced oxidative stress, endothelial dysfunction or the potential role in favoring infection. Further, IV iron administration has been associated with an increased risk of hypotension, headaches or hypersensitivity reactions. Labile iron, which is the iron that is freed into the circulation after administration and non-bound to transferrin, is an important cause of such adverse reactions.
Also Check: What Is Kidney Pain Like
Is It Ok To Take An Iron Supplement Every Day
For the treatment of iron deficiency anemia in adults, 100 to 200 mg of elemental iron per day has been recommended. The best way to take the supplement so that you absorb the greatest amount of iron is to take it in two or more doses during the day. However, extended-release iron products may be taken once a day.
Prevalence Of Anemia Of Chronic Disease And Ckd
In general, anemia is more common in women, in particular, those in their childbearing years. In the latter decades of life, anemia tends to occur without any particular sex predilection. However, in patients with chronic kidney disease , the risk of developing anemia is 30% higher in males than in females. Although males have higher hemoglobin values, they also have higher rates of advanced CKD. The prevalence of anemia is lower in current smokers, which has been attributed to secondary erythrocytosis.
Anemia is common in patients with CKD. The landmark study by Obrador et al showed that among predialysis patients, 68% of those with advanced CKD who required renal replacement therapy had a hematocrit of less than 30% of those, 51% had a hematocrit less than 28%. A review of National Health and Nutrtion Examination Survey data determined that the prevalence of anemia increased with stage of CKD, as follows :
- Stage 1: 8.4%
Don’t Miss: How Do Doctors Remove Kidney Stones
Treatment Of Iron Deficiency Anemia In Dialysis Ckd
CKD patients who are treated with dialysis are especially vulnerable to iron deficiency anemia, due to blood retained in the dialysis machine and tubes .
In contrast to CKD stage 35, for which KDIGO clinical practice guidelines allow a trial of oral iron before starting i.v. iron, these guidelines are very clear regarding therapy for CKD-5D, stating that patients with CKD-5D with anemia should be treated with i.v. iron . This unequivocal recommendation was adopted by the KDOQI , the NICE , and the EBRP position statement and it was based on several RCT and a meta-analysis involving hemodialysis patients in whom a greater increase in Hb was achieved with i.v. iron compared to oral iron, regardless of ESA treatment . The convenience of having a venous access for i.v. iron treatment further supports the choice of an i.v. route.
The guidelines were published in 2012 and 2013, and since then additional studies addressing this subject have been conducted and published, further supporting the use of i.v. iron in CKD-5D. In the meta-analysis by our group, which was previously mentioned, 11 trials with 818 CKD-5D patients were included. It showed that i.v. iron treatment is more likely to achieve a response > 1 g/dL Hb. There were no significant differences regarding mortality or adverse effects .
The recommended treatment is an initial loading dose of 1,000 mg of i.v. iron , followed by maintenance treatment which consists of smaller, regularly administrated, i.v. iron.
Outcomes Of Iron Deficiency Anemia In Ckd
Anemia in CKD has been shown to be associated with an increased risk of morbidity and mortality . In a large observational study, 27,998 patients with CKD were followed up for approximately 5.5 years . The authors reported a higher baseline prevalence of anemia in patients who died than in those who survived . Furthermore, the increase in the prevalence of anemia over the observation period was greatest in those who died despite a shorter period of observation.
The high rates of heart disease and anemia in those who died suggest that anemia accelerates the progression of heart disease and increases the risk of death. However, anemia may be a marker for severity of CKD rather than a causative factor .
A retrospective cohort study among patients with incident CKD who had hemoglobin measurements, in a large health maintenance organization administrative data set, evaluated 5,885 patients . Anemia was found to be a predictor of excess mortality, excess cardiovascular hospitalizations, and excess end-stage renal disease . For those with the most severe anemia , there was an increased rate of mortality , cardiovascular hospitalizations , and ESRD when compared to those who were not anemic.
You May Like: Can Women Pass Kidney Stones
Treatment With Erythropoiesis Stimulating Agents
Guideline 3.1 – treatment of Anaemia – Erythropoiesis stimulating agents
We recommend that treatment with Erythropoiesis Stimulating Agents should be offered to patients with anaemia of CKD who are likely to benefit in terms of quality of life and physical function and to avoid blood transfusion especially in patients considered suitable for transplantation.
Guideline 3.2 – treatment of Anaemia – choice of ESA
We recommend that the decision on the choice of ESA is based on local availability of ESAs.
Guideline 3.3 – treatment of Anaemia with ESA therapy – target Hb
We suggest that patients with CKD on ESA therapy should achieve Hb between:
-
100 and 120 g/L in adults, young people and children aged 2 years and older
-
95 and 115 g/L in children younger than 2 years of age (reflecting the lower normal range in that age
Guideline 3.4 – treatment of Anaemia without ESA therapy – target Hb
We suggest that this Hb target range applies exclusively to patients receiving ESA and are not intended to apply to the treatment of iron deficiency in patients receiving iron therapy without the use of ESAs.
Guideline 3.5 – treatment of Anaemia – initial ESA dose
We recommend that the initial ESA dose should be determined by the patients Hb level, the target Hb level, the observed rate of increase in Hb level and clinical circumstances.
Guideline 3.6 – treatment of Anaemia with ESA therapy – route of administration
Guideline 3.8 – treatment of Anaemia with ESA therapy – ESA dose adjustments
Albuminuria A Risk Factor For Anemia In Chronic Kidney Disease
In a recent study researchers found albuminuria to be a risk factor for anemia in chronic kidney disease. Researchers looked at anemia, albuminuria and glomerular filtration rate . Albuminuria is when albumin is found in the urine, which is a common sign of kidney disease.
The rates of anemia were 43 percent higher in those with albumin-to-creatinine ratio 30 to 299 mg/g and 86 percent higher with ACR above 300 mg/g.
Due to the research being a cross-sectional study, researchers were unable to determine the exact relationship between albuminuria and anemia.
Don’t Miss: Can Blood Test Detect Kidney Failure