Functional Structure Of The Kidneys
nephrons
1. The tubule begins with a hollow enlargement called Bowman’s capsule, which is where water and solutes initially enter the tubule from the bloodstream. This process is known as filtration. The structure comprised of Bowman’s capsule and associated capillaries is called the renal corpuscle.
2. From Bowman’s capsule the tubular fluid flows towards the proximal tubule, which remains in the outer layer of the kidney. The proximal tubule is the major site of reabsorption of water and solutes in equal proportions from the filtered tubular fluid.
3. Then the tubule dips into the hairpin loop of Henle, which descends toward the center of the kidney and then rises back to the cortex. The loop of Henle is also a major site of reabsorption, but unlike the proximal tubule, proportionately more solute than water is reabsorbed, so the tubular fluid is dilute relative to plasma by the end of this segment.
4. The next segment is the distal tubule, which like the proximal tubule remains in the cortex. Both reabsorption and secretion take place in this segment, which is where sodium and potassium concentrations and the pH of the tubular fluid are adjusted to ensure homeostasis.
1. An afferent arteriole takes blood to the renal corpuscle, where the blood passes through the first capillary bed, a ball-shape tuft known as the glomerulus.
2. An efferent arteriole takes blood away from the glomerulus.
How To Maintain Human Homeostasis
While you dont need to do much to know how to maintain homeostasis, its a good idea to keep certain points in mind so that you allow your body to have the right tools to do the job it needs to naturally. Hormones help regulate the chemicals in the body. Based on caloric intake, you can inadvertently alter the chemical composition of your body, forcing it to make adjustments that it shouldnt have to.
When this happens, it may be unable to regulate other aspects of your system properly. Consuming the proper number of calories for your body weight, height, and physical activity is important. Consuming too little can leave your body weak. Consuming too many, and you can alter the chemical composition.
As previously mentioned, if you constantly consumed highly processed, high sugar foods, the likelihood of your body maintaining a healthy blood sugar long-term is diminished. Once that homeostatic mechanism has been compromised beyond repair, you are left with diabetes and all the health issues that come with the diagnosis.
The number, type, and quantity of toxins in your body also affect human homeostasis. When you drink cola or other non-natural beverages, such as alcohol or energy drinks, you introduce toxins to your body that are not intended to be there. This tends to increase the excretory processes in your body, failing your body to regulate properly.
How Does Adh Maintain Homeostasis
4.5/5homeostasishomeostasisADHmore about it
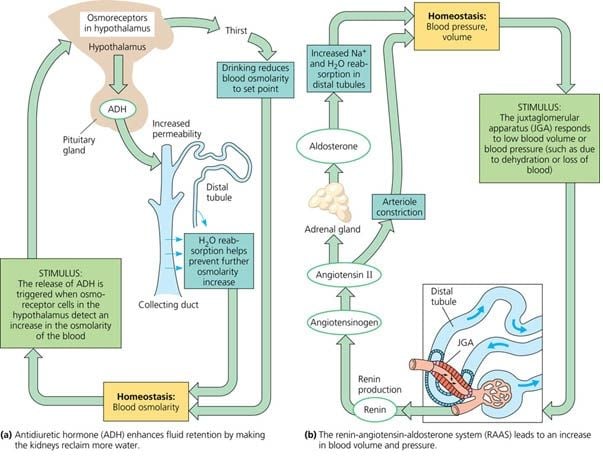
The kidneys can adjust the concentration of the urine to reflect the body’s water needs, conserving water if the body is dehydrated or making urine more dilute to expel excess water when necessary. ADH is a hormone that helps the body to retain water by increasing water reabsorption by the kidneys.
Likewise, how does the kidney maintain homeostasis? The kidneys remove waste products from metabolism such as urea, uric acid, and creatinine by producing and secreting urine. The kidneys help maintain homeostasis by regulating the concentration and volume of body fluids. For example, the amount of H+ and HCO3- secreted by the kidneys controls the body’s pH.
Beside above, how does ADH regulate water concentration levels in the body?
Antidiuretic hormone binds to receptors on cells in the collecting ducts of the kidney and promotes reabsorption of water back into the circulation. These channels transport solute-free water through tubular cells and back into blood, leading to a decrease in plasma osmolarity and an increase osmolarity of urine.
What is water balance and why is it important for homeostasis?
Water is an essential feature of homeostasis in an organism. Water increases the volume of blood, which affects blood pressure and heart rate. Water dissolves gases and allow for efficient exchange and transport of oxygen and carbon dioxide.
Also Check: Seltzer Water Kidney Stones
Homeostasis And The Kidneys
The Big Idea
Homeostasis & the Kidney
- Kidneys play an important role in helping the body maintain homeostasis. They have many important functions:
-
Filter harmful waste products from the blood and drain them out by urine.
-
Balance the level of fluids and salts in the body.
-
Control blood pressure.
-
Help make red blood cells.
The Essential Questions:
- How do the kidneys help the body maintain homeostasis?
- Why is it important for the kidneys to help the body maintain homeostasis?
- What happens if the kidneys stop working?
Justification for Selection of Content:
- Students previously scored poorly on standardized tests, end-of term test or any other test given in the school or district on this content.
- Misconceptions regarding this content are prevalent.
- Content is suited well for teaching via CBL and EDP pedagogies.
The Hook:
- Discuss that March is Kidney Awareness Month! Maybe do unit in March?
- Contact The National Kidney Foundation in Cincinnati Marcia Hilditch to schedule a speaker
- Different body structures are made up of the same type of cells.
- The cell is a permeable membrane.
- Kidney disease is for older people.
- There is a cure for kidney disease.
Unit Lessons and Activities:
- Discuss that March is Kidney Awareness Month! Maybe do unit in March?
- Contact The National Kidney Foundation in Cincinnati Marcia Hilditch to schedule a speaker
- Activity 3: Osmosis & Diffusion Lab 6.1.03e
Lesson 2:
- Activity 1: Cell Membrane Lab 6.2.01f
-
Hook: Rubber Egg Observations
-
Bubble Membrane Activity
What Do The Kidneys Do
Humans have two kidneys. They are complex organs that are vital for life. The kidneys produce urine which is made up of waste products, excess mineral ions and excess water from the body.
Your body is made up of millions of cells. For them to work properly, the conditions inside your body need to be as constant as possible. However everything you do tends to change your internal conditions. You take millions of new molecules into your body when you eat and digest food, you release heat energy every time you move about, the amount of water you take into and lose from your body varies all the time and your cells are constantly producing poisonous waste.
Homeostasis describes the functions of your body which work to keep your internal environment constant within a very narrow range. One of your most important organs of homeostasis is the kidney.
Contents
Also Check: What Std Messes With Your Kidneys
What Are Some Of The Causes Of Chronic Kidney Disease
Chronic kidney disease is defined as having some type of kidney abnormality, or “marker”, such as protein in the urine and having decreased kidney function for three months or longer.
There are many causes of chronic kidney disease. The kidneys may be affected by diseases such as diabetes and high blood pressure. Some kidney conditions are inherited .
Others are congenital that is, individuals may be born with an abnormality that can affect their kidneys. The following are some of the most common types and causes of kidney damage.
Diabetes is a disease in which your body does not make enough insulin or cannot use normal amounts of insulin properly. This results in a high blood sugar level, which can cause problems in many parts of your body. Diabetes is the leading cause of kidney disease.
High blood pressure is another common cause of kidney disease and other complications such as heart attacks and strokes. High blood pressure occurs when the force of blood against your artery walls increases. When high blood pressure is controlled, the risk of complications such as chronic kidney disease is decreased.
Glomerulonephritis is a disease that causes inflammation of the kidney’s tiny filtering units called the glomeruli. Glomerulonephritis may happen suddenly, for example, after a strep throat, and the individual may get well again.However, the disease may develop slowly over several years and it may cause progressive loss of kidney function.
How The Urinary System Works Step By Step
From the kidneys, urine travels down two thin tubes called ureters to the bladder. The ureters are about 8 to 10 inches long. Muscles in the ureter walls constantly tighten and relax to force urine downward away from the kidneys. If urine is allowed to stand still, or back up, a kidney infection can develop.
Don’t Miss: Cranberry Good For Liver
Storage And Excretion Of Wastes
After urine has been produced by the kidneys, it is transported through the ureters to the urinary bladder. The urinary bladder fills with urine and stores it until the body is ready for its excretion. When the volume of the urinary bladder reaches anywhere from 150 to 400 milliliters, its walls begin to stretch and stretch receptors in its walls send signals to the brain and spinal cord. These signals result in the relaxation of the involuntary internal urethral sphincter and the sensation of needing to urinate. Urination may be delayed as long as the bladder does not exceed its maximum volume, but increasing nerve signals lead to greater discomfort and desire to urinate.
Urination is the process of releasing urine from the urinary bladder through the urethra and out of the body. The process of urination begins when the muscles of the urethral sphincters relax, allowing urine to pass through the urethra. At the same time that the sphincters relax, the smooth muscle in the walls of the urinary bladder contract to expel urine from the bladder.
Role Of The Proximal Tubule In Acid
Schematic illustration of acid-base handling in the renal proximal tubules. H+ ions secreted by the proximal tubules via Na+/H+ exchanger 3 combine with filtered bicarbonate to form H2CO3. Through the action of carbonic anhydrase IV and II, the filtered bicarbonate gets reabsorbed back into the blood via electrogenic sodium bicarbonate cotransporter 1 on the basolateral side. Upon stimulation, several proteins such as calcium-sensing receptor , proline-rich tyrosine kinase 2 , and G protein-coupled receptor family C group 5 member C can influence NHE3 activity, thereby modulating acid-base homeostasis. TWIK-related acid-sensitive K+ channel 2 is essential for maintaining basolateral membrane potential, and its absence affects bicarbonate reabsorption in the proximal tubules.
Also Check: Is Honey Good For Your Kidney
How Do Kidneys And The Urinary System Maintain Homeostasis In Humans
The kidneys remove waste products from metabolism such as urea, uric acid, and creatinine by producing and secreting urine. Urine may also contain sulfate and phenol waste and excess sodium, potassium, and chloride ions. The kidneys help maintain homeostasis by regulating the concentration and volume of body fluids.
How Does Osmotic Pressure Of A Plant Cell Is Maintained
Turgor pressure within cells is regulated by osmosis and this also causes the cell wall to expand during growth. One mechanism in plants that regulate turgor pressure is its semipermeable membrane, which only allows some solutes to travel in and out of the cell, which can also maintain a minimum amount of pressure.
Read Also: Wine For Kidney Stones
What Is The Role Of Glucose Homeostasis In Renal Glucosuria
- Author: Rajendra Bhimma, MBChB, MD, PhD, DCH , FCP, MMed Chief Editor: Craig B Langman, MD
The kidneys play an important role in glucose homeostasis. It helps to maintain glucose homeostasis by at least two mechanisms.
-
Under normal circumstances, the kidney filters and reabsorbs 100% of glucose, approximately 180 g of glucose, each day. The glucose transporters expressed in the renal proximal tubule ensure that less than 0.5 g/day is excreted in the urine of healthy adults. More water than glucose is reabsorbed resulting in an increase in the glucose concentration in the urine along the tubule. Consequently the affinity of the transporters for glucose along the tubule increases to allow for complete reabsorption of glucose from the urine.
-
It produces glucose by gluconeogenesis. The key enzymes of gluconeogenesis are phosphoenolpyruvate carboxykinase and glucose 6-phosphatase . These are expressed in the renal proximal tubule only and not the renal medulla. The kidneys produce between 2.0-2.5umol of glucose/kg/min thereby contributing about 20-25% of circulating glucose.
Gluconeogenesis in the kidneys exceeds renal glucose consumption. It is important in the prevention of hypoglycemia, and its inappropriate increase in diabetic patients contributes to the development of hyperglycemia.
References
De Marchi S, Cecchin E, Basile A, Proto G, Donadon W, Jengo A, et al. Close genetic linkage between HLA and renal glycosuria. Am J Nephrol. 1984. 4 :280-6. .
The Urinary System And Homeostasis
- Describe the role of the kidneys in vitamin D activation
- Describe the role of the kidneys in regulating erythropoiesis
- Provide specific examples to demonstrate how the urinary system responds to maintain homeostasis in the body
- Explain how the urinary system relates to other body systems in maintaining homeostasis
- Predict factors or situations affecting the urinary system that could disrupt homeostasis
- Predict the types of problems that would occur in the body if the urinary system could not maintain homeostasis
All systems of the body are interrelated. A change in one system may affect all other systems in the body, with mild to devastating effects. A failure of urinary continence can be embarrassing and inconvenient, but is not life threatening. The loss of other urinary functions may prove fatal. A failure to synthesize vitamin D is one such example.
Vitamin D Synthesis
Erythropoiesis
Blood Pressure Regulation
The Enzyme Renin Converts the Pro-enzyme Angiotensin
Figure 1
Regulation of Osmolarity
Recovery of Electrolytes
Sodium, calcium, and potassium must be closely regulated. The role of Na+ and Ca++ homeostasis has been discussed at length. Failure of K+ regulation can have serious consequences on nerve conduction, skeletal muscle function, and most significantly, on cardiac muscle contraction and rhythm.
pH Regulation
Everyday Connection
Stem Cells and Repair of Kidney Damage
Chapter Review
Reference
Review Questions
Recommended Reading: Osteocleanse
The Role Of The Kidney In Glucose Homeostasis
Submitted: May 1st 2014Reviewed: September 10th 2014Published: April 1st 2015
DOI: 10.5772/59173
- Department of Diabetes, Nutrition, Metabolic Diseases, University of Medicine and Pharmacy Craiova, Romania
Eugen Mota
Ilie-Robert Dinu
DOI: 10.5772/59173
Everyday Connections: Stem Cells And Repair Of Kidney Damage
Stem cells are unspecialized cells that can reproduce themselves via cell division, sometimes after years of inactivity. Under certain conditions, they may differentiate into tissue-specific or organ-specific cells with special functions. In some cases, stem cells may continually divide to produce a mature cell and to replace themselves. Stem cell therapy has an enormous potential to improve the quality of life or save the lives of people suffering from debilitating or life-threatening diseases. There have been several studies in animals, but since stem cell therapy is still in its infancy, there have been limited experiments in humans.
Acute kidney injury can be caused by a number of factors, including transplants and other surgeries. It affects 710 percent of all hospitalized patients, resulting in the deaths of 3540 percent of inpatients. In limited studies using mesenchymal stem cells, there have been fewer instances of kidney damage after surgery, the length of hospital stays has been reduced, and there have been fewer readmissions after release.
How do these stem cells work to protect or repair the kidney? Scientists are unsure at this point, but some evidence has shown that these stem cells release several growth factors in endocrine and paracrine ways. As further studies are conducted to assess the safety and effectiveness of stem cell therapy, we will move closer to a day when kidney injury is rare, and curative treatments are routine.
Don’t Miss: Is Honey Good For Kidney
Regulation Of Hco3 Reabsorption In The Proximal Tubule
A number of processes regulate proximal tubule HCO3 reabsorption both acutely and chronically. Many of these regulatory processes function to maintain acid-base homeostasis and are seemingly quite redundant this is true in both the proximal and distal nephron segments. However, other processes overlap with volume or sodium regulatory processes, and the acid-base effects seem secondary and at times, dysfunctional for pH per se for instance, during metabolic alkalosis induced by vomiting and volume depletion, various hormones are activated that restore volume status but secondarily maintain high plasma HCO3 and alkalemia.
Despite the regulation mentioned above, changes in proximal HCO3 reabsorption may not be directly reflected in changes in wholekidney net acid excretion or urinary HCO3 excretion, because additional HCO3 reabsorption and acid secretion occur in the distal nephron. Also, because virtually all of filtered HCO3 is normally reabsorbed by the kidneys, increases in HCO3 reabsorption per se cannot compensate for increased systemic acid loads This compensation can only occur with increased acid excretion as titratable acids or NH4+.
The Kidney In Diabetes Mellitus
All the metabolic pathways regarding the involvement of the kidney in glucose homeostasis are modified in subjects with diabetes mellitus. Subjects with type 2 diabetes mellitus have an increased renal release of glucose into the circulation in the fasting state . Although one can think that the liver determines increased glucose release into the circulation in diabetes, the liver and the kidneys have comparable increase in renal glucose release . The kidney can increase its glucose production with 300% compared with the liver that can increase gluconeogenesis only by 30%. Gluconeogenesis, in the kidney, could explain this glucose increase, in the fasting state .
Both renal glucose uptake and glucose production are increased in both the postprandial and post-absorptive states in diabetic patients .
It is well known that glucosuria in diabetic patients occurs at different plasma glucose levels compared with the levels where glucosuria can occur in non-diabetic individuals . This is determined by the increased glucose reabsorbtion in subjects with diabetes mellitus. Therefore, the Tm for glucose is increased and glucosuria may occur at higher than normal blood glucose levels. Several studies indicated that the Tm increased from near 350 mg min in subjects with normal glucose tolerance to approximately 420 mgmin in subjects with diabetes mellitus .
You May Like: Does Kidney Infection Cause Diarrhea