Blood Volume Will Fall
I showed you elsewhere that if diet sodium goes down kidney losses continue at the higher level for several days. As a result some sodium is lost from the body. Almost all of that loss is from the fluid outside the cells, and normal cell function requires that sodium concentration stays constant at 140 mEq/l. Therefore, loss of sodium is loss of fluid. We all know we lose weight if we cut down our salt intake.
Less fluid volume includes less blood volume, so the volume pumped by the heart will go down. Blood pressure tends to go down, as well. This should lower GFR.
What Is Urine Made Of
Urine is made of water, urea, electrolytes, and other waste products. The exact contents of urine vary depending on how much fluid and salt you take in, your environment, and your health. Some medicines and drugs are also excreted in urine and can be found in the urine.
- 94% water
- .1% uric acid
*Electrolytes
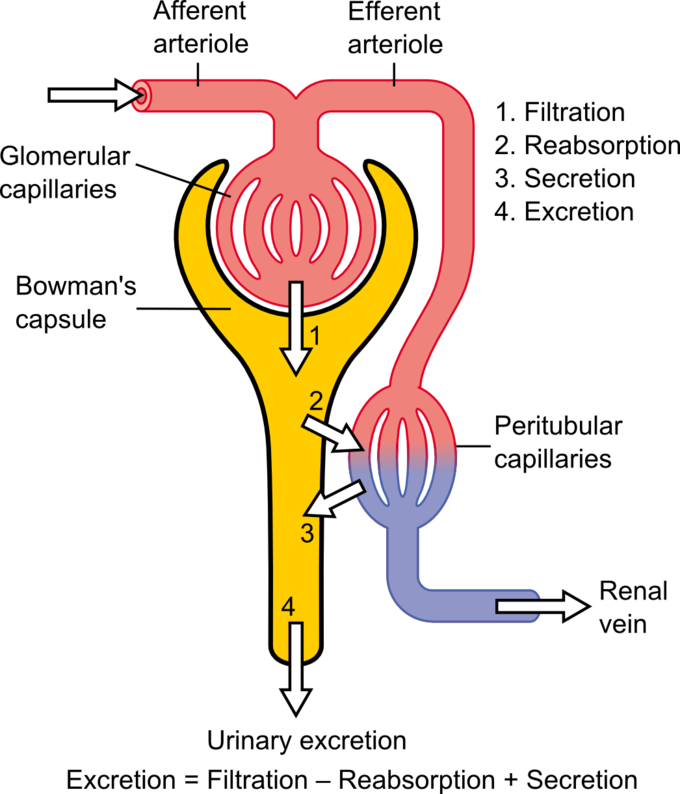
As mentioned prior, urine is formed in the nephrons by a three-step process: glomerular filtration, tubular re-absorption, and tubular secretion. The amount of urine varies based on fluid intake and ones environment.
The Glomerulus Filters Water And Other Substances From The Bloodstream
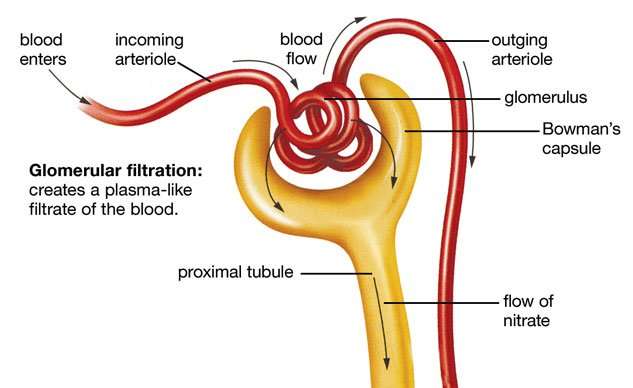
Each kidney contains over 1 million tiny structures called nephrons. Each nephron has a glomerulus, the site of blood filtration. The glomerulus is a network of capillaries surrounded by a cuplike structure, the glomerular capsule . As blood flows through the glomerulus, blood pressure pushes water and solutes from the capillaries into the capsule through a filtration membrane. This glomerular filtration begins the urine formation process.
Recommended Reading: Constipation Or Kidney Stone
Extrinsic Controls: Neural And Hormonal Mechanisms
The extrinsic control mechanisms have an effect on GFR, but their primary function is to maintain systemic blood pressure. While the intrinsic controls functioned to specifically control GFR at the level of the kidneys, the neural and hormonal controls have a broader scope and function to meet the whole bodys needs, not just the needs of the kidneys.
This Is A Very Simplified Overview
The real sources and regulation of A2, how it works in the kidneys, where it is made in the kidneys, how it can get into the circulation, all that, is a massive story. Likewise the mechanisms of filtration itself and tubuloglomerular feedback.
For fairness to the more ambitious or technically trained, here are some reasonable introductions to where things are. My favorite reviews are by mathematical modelers. I call them meta analysts with brains. They pull together what pathways are thought to work along with lists of the key transfer constants, model them with correct mathematics, and see if things match to reality.
Here are two about angiotensin 2: Part One Part two
Here is a brilliant author on filtration itself: Modeling glomerular filtration.
Also Check: Celery Juice And Kidney Disease
True Gfr Inulin Clearance
Inulin is a large carbohydrate polymer that lacks the one defect of creatinine. After filtration the nephron cells neither reabsorb it back into the blood nor secrete it from blood into the tubule fluid. It passes as through a glass tube. So the clearance of inulin is GFR.
Given this perfect marker, how bad a marker is creatinine?
Jacob Lemann, a great scientist and a close friend, left behind at his death the lab books of his experiments. We had the good fortune to get copies made, page by page. From these we copied out multiple instances where he measured both inulin and creatinine clearances. I made this graph to compare them.
First, take a look at the axes. GFR values are in hundreds of ml/min. Five ml fill a teaspoon, 15 ml fill a tablespoon, 30 ml is a shot of whiskey. The two kidneys can filter a lot out of blood every minute, enough to fill 3 4 shot glasses, or more.
The diagonal line marks a one to one correspondence. Most of the points lie above it. This reflects the secretion of creatinine by OAT-1. CCr overestimates GFR. But CCr moves in parallel with the true GFR and therefore is useful.
The dashed reference lines lie at the medians for inulin and creatinine clearance . As an estimate, therefore, CCr overestimates CIn by about 128/112 or 11%. That overestimate from secretion is clearly due to a constant secretion acting as the intercept of the linear regression of CCr on Cin.
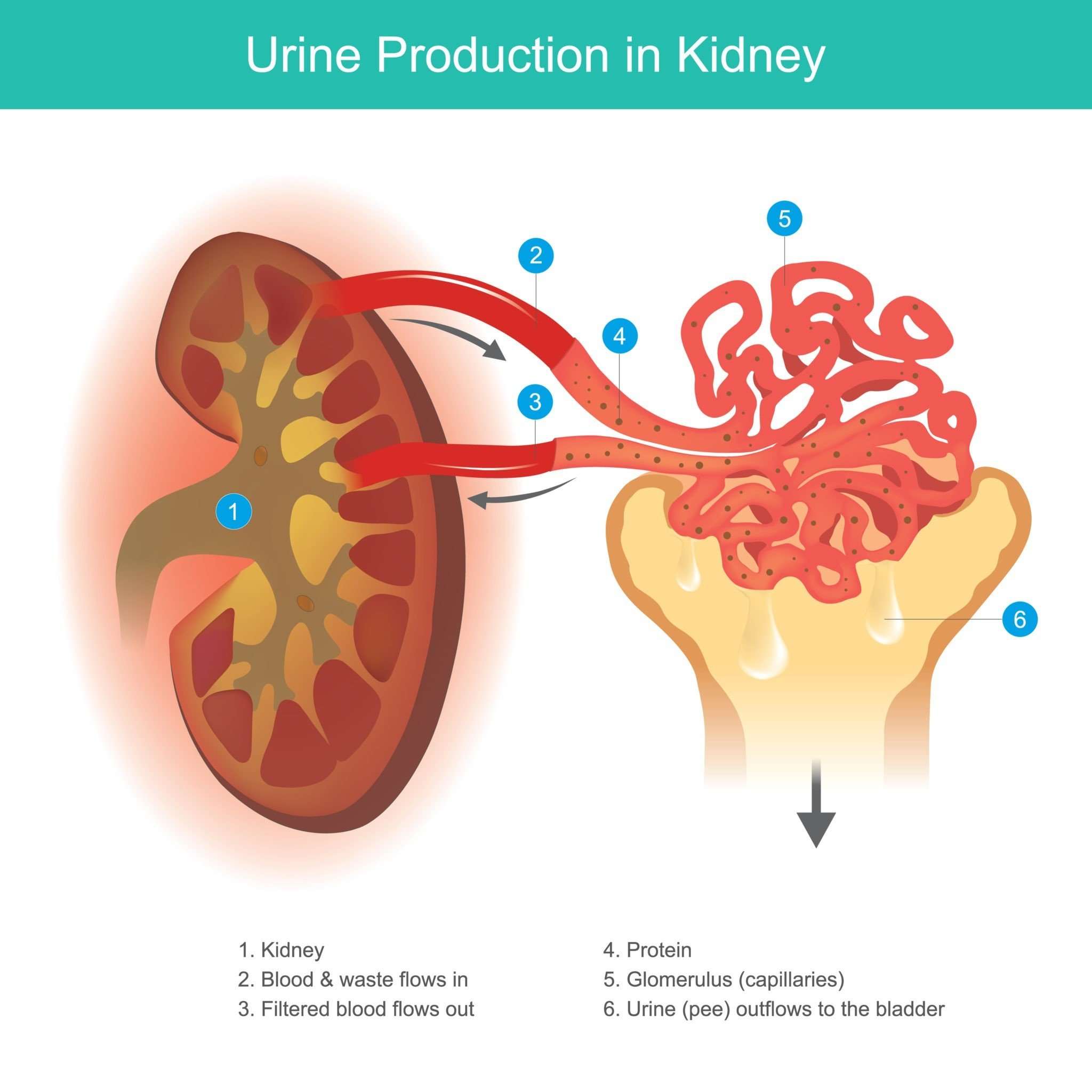
Where Are The Kidneys And How Do They Function
There are two kidneys, each about the size of a fist, located on either side of the spine at the lowest level of the rib cage. Each kidney contains up to a million functioning units called nephrons. A nephron consists of a filtering unit of tiny blood vessels called a glomerulus attached to a tubule. When blood enters the glomerulus, it is filtered and the remaining fluid then passes along the tubule. In the tubule, chemicals and water are either added to or removed from this filtered fluid according to the body’s needs, the final product being the urine we excrete.
The kidneys perform their life-sustaining job of filtering and returning to the bloodstream about 200 quarts of fluid every 24 hours. About two quarts are removed from the body in the form of urine, and about 198 quarts are recovered. The urine we excrete has been stored in the bladder for anywhere from 1 to 8 hours.
You May Like: Is Celery Juice Good For Your Kidneys
What Clinical Trials Are Open
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health. The NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
What Are The Parts Of The Urinary Tract
People usually have two kidneys, but can live a normal, healthy life with just one. The kidneys are under the ribcage in the back, one on each side. Each adult kidney is about the size of a fist.
Each kidney has an outer layer called the cortex, which contains filtering units. The center part of the kidney, the medulla , has fan-shaped structures called pyramids. These drain urine into cup-shaped tubes called calyxes .
From the calyxes, pee travels out of the kidneys through the ureters to be stored in the bladder . When a person urinates, the pee exits the bladder and goes out of the body through the urethra , another tube-like structure. The male urethra ends at the tip of the penis the female urethra ends just above the vaginal opening.
Don’t Miss: Cranberry Juice Good For Liver
What Is Glomerular Filtrate Composed Of
4.9/5filtrateGlomerular filtratequestion here
The glomerular filtrate contains water, glucose, salts, and urea, so the first option is wrong. The glucose, salts, and urea enter the Bowman’s capsule in essentially the same concentrations as they have in the blood.
Likewise, what is found in filtrate? Normal filtrate contains of water, glucose, amino acids, urea, creatinine, and solutes such as sodium chloride, calcium, potassium and bicarbonate ions. Proteins or red blood cells are not present in the filtrate because they are too large to pass through the glomerular filtration membrane.
Keeping this in consideration, what makes up the glomerular filtration membrane?
Structure of the Filtration MembraneThere are three layers that make up the filtration membrane: two epithelia and the basement membrane that lies between them. The next layer is the glomerular basement membrane, a shared basement membrane between the two epithelia .
How glomerular filtrate is formed?
Glomerular Filtration. Filtrate is produced by the glomerulus when the hydrostatic pressure produced by the heart pushes water and solutes through the filtration membrane. Glomerular filtration is a passive process as cellular energy is not used at the filtration membrane to produce filtrate.
Capillary Network Within The Nephron
The capillary network that originates from the renal arteries supplies the nephron with blood that needs to be filtered. The branch that enters the glomerulus is called the afferent arteriole. The branch that exits the glomerulus is called the efferent arteriole. Within the glomerulus, the network of capillaries is called the glomerular capillary bed. Once the efferent arteriole exits the glomerulus, it forms the peritubular capillary network, which surrounds and interacts with parts of the renal tubule. In cortical nephrons, the peritubular capillary network surrounds the PCT and DCT. In juxtamedullary nephrons, the peritubular capillary network forms a network around the loop of Henle and is called the vasa recta.
Don’t Miss: Is Watermelon Good For Kidney Patients
What Is The Difference Between Filtrate And Urine
The main difference between filtrate and urine is that filtrate is the liquid filtered out from the blood into Bowmans capsule whereas urine is the nitrogenous liquid formed by the nephron, the functional unit of the kidney.
Filtrate and urine are two types of liquids produced inside the kidney as a result of the kidney function. Furthermore, the filtrate is similar in composition to blood plasma, but it does not contain globular proteins and other large molecules while urine mainly contains the waste products of the body, excess ions, and water.
Reabsorption Moves Nutrients And Water Back Into The Bloodstream
The glomerulus filters water and small solutes out of the bloodstream. The resulting filtrate contains waste, but also other substances the body needs: essential ions, glucose, amino acids, and smaller proteins. When the filtrate exits the glomerulus, it flows into a duct in the nephron called the renal tubule. As it moves, the needed substances and some water are reabsorbed through the tube wall into adjacent capillaries. This reabsorption of vital nutrients from the filtrate is the second step in urine creation.
Read Also: Orange Juice Renal Diet
Slit Diaphragm: A Size
As early as 1972, Karnovsky and Ainsworth presented evidence for the podocyte slit diaphragm being the size-selective molecular sieve, as demonstrated by using large tracer markers. Furthermore, based on electron microscopic findings, Rodewald and Karnovsky proposed that the slit diaphragm has an ordered structure with pores smaller than albumin. However, direct evidence for a filter function of the slit diaphragm was not shown, and knowledge about its molecular composition remained obscure until recently. In 1998, Kestilä et al. isolated the gene mutated in congenital nephrotic syndrome of the Finnish type , a rare autosomal recessive disease characterized by massive nonselective proteinuria at birth and lack of a podocyte slit diaphragm. The disease gene was shown to encode a novel protein named nephrin, which in the kidney is solely located in glomerular podocytes. Nephrin was the first known protein to be localized, via immunoelectron microscopy, to the slit diaphragm . Inactivation of the gene in mice leads to massive proteinuria, absence of a slit diaphragm, and neonatal death .
How Is Urine Produced In The Kidneys
Urine is produced and processed in functional and structural units of the kidney that are nephrons.
Explanation:
Nephron filters the blood then it reabsorbs all the useful substances from that filtrate and removes the rest in the form of urine.
Following steps are involved in formation of urine in nephron:
Ultrafiltration
- Blood enters the nephron through afferent arteriole and flows into the glomerulus.
-
Now this blood has both filterable blood components and non-filterable blood components. The walls of glomerulus are porous which provide necessary filtration pressure.
-
Filterable blood components i.e water, nitrogenous waste, nutrients and salts move toward the inside of the glomerulus and take a plasma like form called glomerular filtrate .
-
On the other hand, non-filterable blood components bypass the filtration process by exiting through the efferent arteriole.
-
Glomerular filtrate essentially contains #color”amino acids, water, sodium chloride, potassium,”# #color”bicarbonate ions, creatinine and urea”# when it leaves glomerulus and enters PCT.
ReabsorptionReabsorption means the movement of stuff from glomerular filtrate back into the blood. Reabsoprtion occurs next to filtration. In this process, several components of the glomelular filtrate that are vital for body functioning are transferred back to the blood. It takes place in PCT, Loop of henle, DCT and collecting duct.
Recommended Reading: Is Grape Juice Good For Kidney Stones
Module : The Urinary System
- Describe the process of filtration and relate it to net filtration pressure.
The process of producing urine occurs in three stages: filtration, reabsorption, and secretion. The physiologic goal is to modify the composition of the blood plasma and, in doing so, eliminate only waste in the form of urine.
It Adapts To Keep Flow Constant
Like all arterioles, but better, the AA dilates when pressure falls reducing tension in its walls. Likewise when pressure rises it contracts. This so called intrinsic autoregulation keeps glomerular capillary flow and pressure more or less constant over a range of pressures and flows delivered to the kidneys by the heart.
Read Also: Is Celery Good For Kidneys
Molecules Filtered And Not Reabsorbed
Because the U/P ratio gives the CCr at a urine volume of one liter per day, if your GFR is 75 l/d instead of 150 l/d, your U/P value at one liter is 75, not 150. The degree to which filtrate is concentrated at one liter per day is half, but all things being otherwise equal, urine concentrations of all substances filtered and not reabsorbed will be the same as at a U/P of 150.
This is because if only filtered, the plasma concentration will double as the GFR falls by half. But unless the supply of molecules falls or rises metabolism, diet the urine concentration at one liter must be unchanged to maintain excretion. The U/P ratio falls because the plasma concentration doubles.
Tubular Reabsorption And Secretion
Tubular reabsorption occurs in the PCT part of the renal tubule. Almost all nutrients are reabsorbed, and this occurs either by passive or active transport. Reabsorption of water and some key electrolytes are regulated and can be influenced by hormones. Sodium is the most abundant ion and most of it is reabsorbed by active transport and then transported to the peritubular capillaries. Because Na+ is actively transported out of the tubule, water follows it to even out the osmotic pressure. Water is also independently reabsorbed into the peritubular capillaries due to the presence of aquaporins, or water channels, in the PCT. This occurs due to the low blood pressure and high osmotic pressure in the peritubular capillaries. However, every solute has a transport maximum and the excess is not reabsorbed.
In the loop of Henle, the permeability of the membrane changes. The descending limb is permeable to water, not solutes the opposite is true for the ascending limb. Additionally, the loop of Henle invades the renal medulla, which is naturally high in salt concentration and tends to absorb water from the renal tubule and concentrate the filtrate. The osmotic gradient increases as it moves deeper into the medulla. Because two sides of the loop of Henle perform opposing functions, as illustrated in Figure 22.8, it acts as a countercurrent multiplier. The vasa recta around it acts as the countercurrent exchanger.
Recommended Reading: Can Wine Cause Kidney Stones
Why Do We Care
Stones may injure kidneys as they obstruct. Surgery may injure kidneys. Kidneys can be lost. So kidney stone patients can lose kidney function. Estimating equations are a clue. If coupled with blood, the 24 hour kidney stone testing will show true creatinine clearance. But that, though in one way more exact than CKD EPI, overestimates true GFR in another creatinine secretion. Most of the time all of the measures will coincide well enough for routine care. Definitive measurements like inulin clearance are not clinically feasible.
Example Question #: Kidney And Nephron Physiology
A renal afferent arteriole has a larger radius than the efferent arteriole. What is the effect of this larger radius on the function of the kidney?
Possible Answers:
Afferent arteriole flow is decreased
Antidiuretic hormone secretion is decreased
Reabsorption in the nephron tubules is increased
Glomerular filtration rate is decreased
Blood flow to the kidney is decreased
Correct answer:
Reabsorption in the nephron tubules is increased
A renal afferent arteriole is directed toward the glomerulus, while a renal efferent arteriole is directed away from the glomerlus. If the radius of the afferent arteriole is increased, there is more flow through it toward the glomerulus, and if there is a smaller radius in the efferent arteriole, there is a resultant back pressure in the glomerulus. This is can be imagined as trying to squeeze a high-pressure hose through a small pipe. This pressure increases the force within the glomerulus to increase filtration, and subsequently increase reabsorption.
Antidiuretic hormone secretion has a neglible effect on the radius of renal arterioles. Blood flow to the kidney is increased when afferent arteriole radius is increased .
Read Also: Constipation Kidney Stones
Example Question #4: Biology
At which point in a nephron would the osmolarity of the filtrate be highest? Assume that antidiuretic hormone is not present in the body.
Possible Answers:
The bottom of the loop of Henle
The proximal convoluted tubule
The bottom of the loop of Henle
It is important to understand how urine is concentrated as it travels through the nephron. The proximal convoluted tubule does not alter the osmolarity of the filtrate, the loop of Henle increases the osmolarity of the filtrate, and the distal convoluted tubule lowers the osmolarity of the filtrate. In the absence of antidiuretic hormone, the collecting duct will be impermeable to water, preventing it from leaving the filtrate and resulting in more dilute urine. With the collecting duct impermeable to water, the filtrate will be most concentrated at the bottom of the loop of Henle.
It Keeps Filtration Constant Under Stress
The final result is a dual regulation. When renal inflow falls, the AA dilates and via renin and A2 constrict the EA. This latter keeps the pressure up in the capillary. So by its own intrinsic autoregulation and by its control of local A2 production, the AA can keep filtration reasonably constant over quite a range of systemic blood pressures and cardiac outputs of blood.
Likewise it transponds stress reactions with sympathetic activity flight or fight into EA constriction so filtration can stay constant even as AA constrict. Finally it permits so called tubulo-glomerular feedback from the JGA so a fall in downstream sodium chloride delivery can trigger off more filtration.
Also Check: Does Red Wine Cause Kidney Stones