Bone Physiology And Pathophysiology
The association of impaired bone status with poor clinical outcomes may reflect one or more of the many functions of bone:
-
physical: body support, facilitation of movement and protection of internal organs against external forces;
-
haematopoiesis: harbours bone marrow, producing blood cells;
-
nutritional: storage of minerals and fat, and indirectly of muscle protein through harbouring skeletal muscles;
-
metabolic: mineral metabolism and acidbase balance; and
-
endocrine and paracrine: bonevascular axis pathways including Wnt signalling, the OPG/receptor activator of nuclear factor-B /RANK ligand system and the Galectin-3/receptor of advanced glycation end products axis.
Cortical and trabecular bone differ as regards their functions, metabolic activity and implications for clinical outcomes.
The location of cortical and trabecular bone should be considered in bone status assessments.
Lower Vitamin D Levels
Many dialysis patients are deficient in vitamin D. They are not eating dairy products, and the specific nephrology vitamins do not contain vitamin D.; Patients often do not get adequate sunlight exposure.; It had been thought that 25-hydroxyvitamin D25Dlevels were not important in patients who were taking calcitriol or vitamin D analogues because they had adequate amounts of the active hormone, and only the kidney had 1-alpha-hydroxylase.;
However, it has been documented that many cells can convert 25D into 1,252D intracellularly without secretion of the 1,252D, so that serum levels did not reflect the actual activity.; This is seen in skeletal muscle, T-cells, and parathyroid cells. The optimal serum level of 25D in dialysis patients is not yet determined, particularly if the patients are receiving analogs, but until ongoing studies are completed, it makes sense to aim for a level of 20 to 50 ng/dL. This is the range associated with the lowest mortality in men and women from the general population.
Bones respond to mechanical forces, and many patients with CKD-stage 4-5 do not get much weight-bearing exercise.; Walking, stair-climbing and dancing, as well as back extension exercises, should be encouraged in these patients. Exercise programs have not been shown to reduce fractures in large trials, but they make a lot of sense and can also improve cardiovascular and mental health.
Fracture Risk Assessment Tool Model
The most important health consequence of osteoporosis is fractures. Recently, algorithms have been developed to predict the risk of fracture in individuals that incorporate significant predictors of fracture risk in addition to BMD. Estimating the 10-year risk of a major osteoporotic fracture , forearm, or proximal humerus) is possible with algorithms that integrate the weight of clinical risk fractures for fracture risk with or without information on the BMD have been developed . They can be used to compute the 10-year probability of hip fracture or a major osteoporotic fracture .
Clinical risk factors used in FRAX are as follows :
-
– Current age
-
– A prior osteoporotic fracture
-
– BMD of femur neck
-
– Low BMI
-
– Oral glucocorticoids 5 mg/d of prednisone for >3 months
-
– Rheumatoid arthritis
-
– Parental history of hip fracture
-
– Secondary causes of osteoporosis: Type-1 DM, early menopause <40 years, etc.
-
– Being a past or current smoker
-
– Alcohol intake
Probabilities have been computed for several countries .
Read Also: How Do Doctors Break Up A Kidney Stone
A Tiny Gland Can Turn Your Whole System Upside Down
About one in 1,000 Americans have primary hyperparathyroidism, three times as many women as men. Its becomes increasingly more common over age 60.
A little background: Primary hyperparathyroidism is not a problem with the thyroid gland. Rather, it affects the tiny pea-size parathyroid glands on or near the thyroid. There are four of them, but usually only one is overactive, signaling excessive release of parathyroid hormone. That hormones purpose is to maintain the right level of calcium in the blood, and when its overactive, it signals the body to pulltoo much calcium from the bones into the bloodstream. That can weaken bones and lead to osteoporosis and fracturescause kidney stonesand create neurological issues that affect concentration and memory and lead to depression.
Until the 1970s, people with primary hyperparathyroidism would be diagnosed when they went to their doctors with serious complaintsbone pain, broken bones, abdominal pain and kidney stones. Since that time, the disease is generally caught earlier through calcium tests, which are now part of the routine blood test you get during an annual physical.
But what if you get the diagnosis after a regular checkup but dont have any symptoms? Should you still get your diseased parathyroid gland removed?
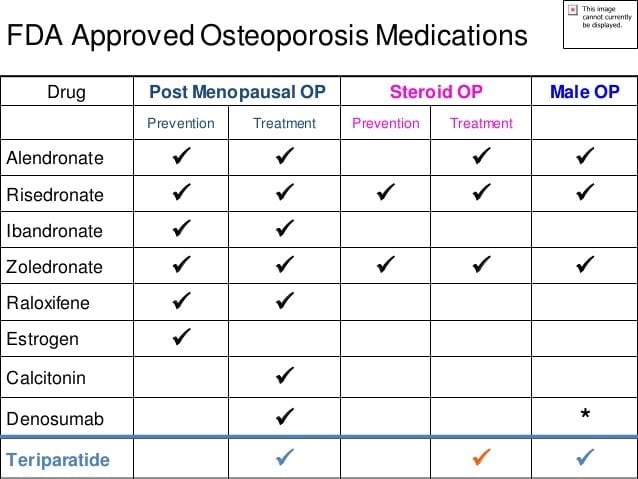
Cautions To Be Taken Contraindications And Complications To Bp Therapy
The absorption of oral BPs is less than 1% with any food, beverage other than plain water, or medications within 2 h after drug administration. Oral BPs should be used with caution: they should not be used in patients with active upper GI diseases, inability to remain upright for 3060 min, anatomic or functional esophageal abnormalities that might delay the transit of the tablet , V-D deficiency, hypocalcemia, and hypersensitivity to drug and kidney failure . Intravenous administration of BPs, such as ibandronate and zoledronate, causes acute phase reactions with the first dose and it can last several days in some patients; this can be prevented by administering acetaminophen. BPs have been reported to cause bone, joint, or muscle complaints; osteonecrosis of the jaw ; and alendronate causing atypical fractures .
Raloxifene has been shown to reduce the risk of fractures of the spine in women with postmenopausal osteoporosis, but its efficacy in reducing non-vertebral or hip fractures has not been demonstrated. Increases in hot flushes are contraindicated in fertile women and those who have had venous thromboembolic disease .
Estrogen replacement therapy is used for the prevention of postmenopausal osteoporosis for those showing a significant risk of osteoporosis and for whom non-estrogen medications are not considered to be appropriate, but estrogen has never been approved for the treatment of osteoporosis.
You May Like: Does Kidney Stone Pain Get Worse At Night
Universal Recommendations For All Patients
Several interventions, including an adequate intake of calcium and V-D, are fundamental aspects for any osteoporosis prevention or treatment program, including lifelong regular weight-bearing and muscle-strengthening exercises, cessation of tobacco use and excess alcohol intake, and treatment of risk factors for falling .
In order to maintain serum calcium at a constant level, an external supply of adequate calcium is necessary; otherwise, low serum calcium levels promote bone resorption to bring the calcium levels to normal. Calcium requirements increase among older persons; thus, the older population is particularly susceptible to calcium deficiency. The Institute of Medicine recommends a daily intake of 1000 mg/day for men aged 5070 years and 1200 mg of calcium for women aged over 50 years and men aged over 70 years .
Vitamin D is necessary for calcium absorption, bone health, muscle performance, and balance. The IOM recommends a dose of 600 IU/day until the age of 70 years in adults and 800 IU/day thereafter . Chief dietary sources of V-D include V-Dfortified milk, juices and cereals, saltwater fish, and liver. Supplementation with V-D2 or V-D3 may be used.
Alcohol
Caffeine
Patients should be advised to limit their caffeine intake to less than 1 to 2 servings of caffeinated drinks per day. Some studies showed that there is a relationship between caffeine consumption and fracture risk .
Exercise
Prevention of falls
Pregnancy And Lactation Associated Osteoporosis
- Temporary decreases in bone density are a normal part of pregnancy and lactationbut fractures during this time are extremely rare.
- Fractures of the spine associated with severe back pain are most commonly described, but PLO can also be associated with hip fractures or other types of fracture.
- In the most common scenario, PLO is discovered after a pregnant or breastfeeding woman develops severe back pain, and imaging reveals multiple vertebral fractures.
- Some women with PLO have a pre-pregnancy diagnosis of osteoporosis, but most women with PLO have not been previously diagnosed with osteoporosis, and never had a bone assessment prior to the onset of symptoms.
Note: This list may not include all of the diseases and conditions that may cause bone loss. Talk to your doctor and ask if any of the conditions you have may be causing bone loss.
Don’t Miss: What Herbs Help The Kidneys
Approach To A Patient With Osteoporosis
A detailed history and physical examination together with BMD assessment, vertebral imaging to diagnose vertebral fractures , and the WHO-defined 10-year estimated fracture probability test are utilized to establish an individual patients fracture risk .
All postmenopausal women and men aged 50 years and above should be evaluated for osteoporosis risk in order to determine the need for BMD testing and/or vertebral imaging. In general, the more the risk factors, larger is the risk of fracture. Osteoporosis is preventable and treatable, but because there are no warning signs prior to a fracture, many people are not being diagnosed in time to receive effective therapy during the early phase of this disease. The factors that increase the risk of osteoporosis-related fractures are listed in .
Worsening Kidney Function Increases Risk Of Osteoporosis
Written byDevon AndrePublished onApril 23, 2018
Osteoporosis is a major concern for adults getting closer to their elderly years. It can lead to severe injury even after a minor fall or abrasion and can cause elderly patients to have decreased mobility.
A common comorbidity of osteoporosis is chronic kidney disease , although the relationship between them doesnt have much research behind it. Adults with CKD face a far higher risk of death with the worsening of the kidneys than adults without CKD.
The connection between CKD and osteoporosis isnt entirely unfounded. CKD is also related to a decrease in bone quality and serious injury after a fall, including bone fractures. A group of researchers recently released the results of their new study, seeking to answer certain questions about CKD and its relationship to osteoporosis.
Specifically, they looked into whether CKD increases the risk of fracture or whether it simply indicates underlying medical concerns and if race or ethnicity affects the results. African Americans have a higher rate of CKD while also reporting lower fracture levels than Caucasians.
Approximately 33 percent of all older adults will suffer an osteoporotic fracture in their lifetime and 25 percent will also develop CKD. The researchers found that even moderate cases of CKD in elderly patients were related to an increased risk of fracture, despite any other morbidities the patient may be suffering.
Don’t Miss: Is Mulberry Good For Kidneys
Associations Of Low Bmd With Vascular Calcification
As discussed below, mechanisms of vascular calcification and bone mineralization share several common pathways, which may explain why low BMD is strongly related to vascular calcification in the general population and in patients with ESRD . Not only low bone mass but also bone loss is an independent predictor for progression of vascular calcification . In a population-based cohort study with 25years follow-up of older men and women, Kiel et al. demonstrated that bone loss at the second metacarpal of the hand as assessed by simple plain radiographs is associated with increased aortic calcification index in women, but not in men. This suggests that endocrine factors such as oestrogen might play a role in the interplay between bone and vasculature. Low trabecular bone volume, as assessed by iliac bone biopsy, has been shown to correlate with the progression of calcification as assessed by CAC, and lower bone turnover was associated with less rapid CAC progression in HD patients . These observations may imply that normalizing bone metabolism could represent an effective option to prevent vascular calcification; however, so far there is no strong clinical evidence confirming that such interventions will reduce established vascular calcification. Also, the crucial mechanism of the bonevascular axis are not fully understood.
Low bone mass and bone loss are linked with vascular calcification.
Management Of Mineral Disorders And Fracture In Ckd
Since the incidence of fracture is high in CKD patients, the prevention of bone and mineral events are crucial and should be a challenge for the different experts involved in patient management. Several guidelines to prevent fractures could be also applied to CKD patients. Falls is a major determinant of fracture that could be prevented, although high incidence of falls is not fully documented in CKD. Factors associated with falls such as low muscle function could be prevented by programs based on exercise in rehabilitation settings with the aim of promoting muscle strength and equilibrium. Denutrition is a factor significantly associated in CKD in dialyzed men with hip fractures . Special attention should be paid to adequate food intake in this context. The prevention strategy should be particularly oriented in the elderly, in whom age comes in addition to mineral disorders. Overall, the correction of serum mineral disorders from the beginning of the decline of kidney function remains a major goal to reduce the comorbidities observed in CKD-MBD.
Proposed algorithm for treatment decision in patients with CKD and fracture. Treatment decisions are dependent of the levels of parathyroid hormone and bone specific alkaline phosphatase levels. The different conditions are shown, to guide treatment decisions appropriately.
Citation: Endocrine Connections 9, 4; 10.1530/EC-20-0039
Clinical Findings And Complications
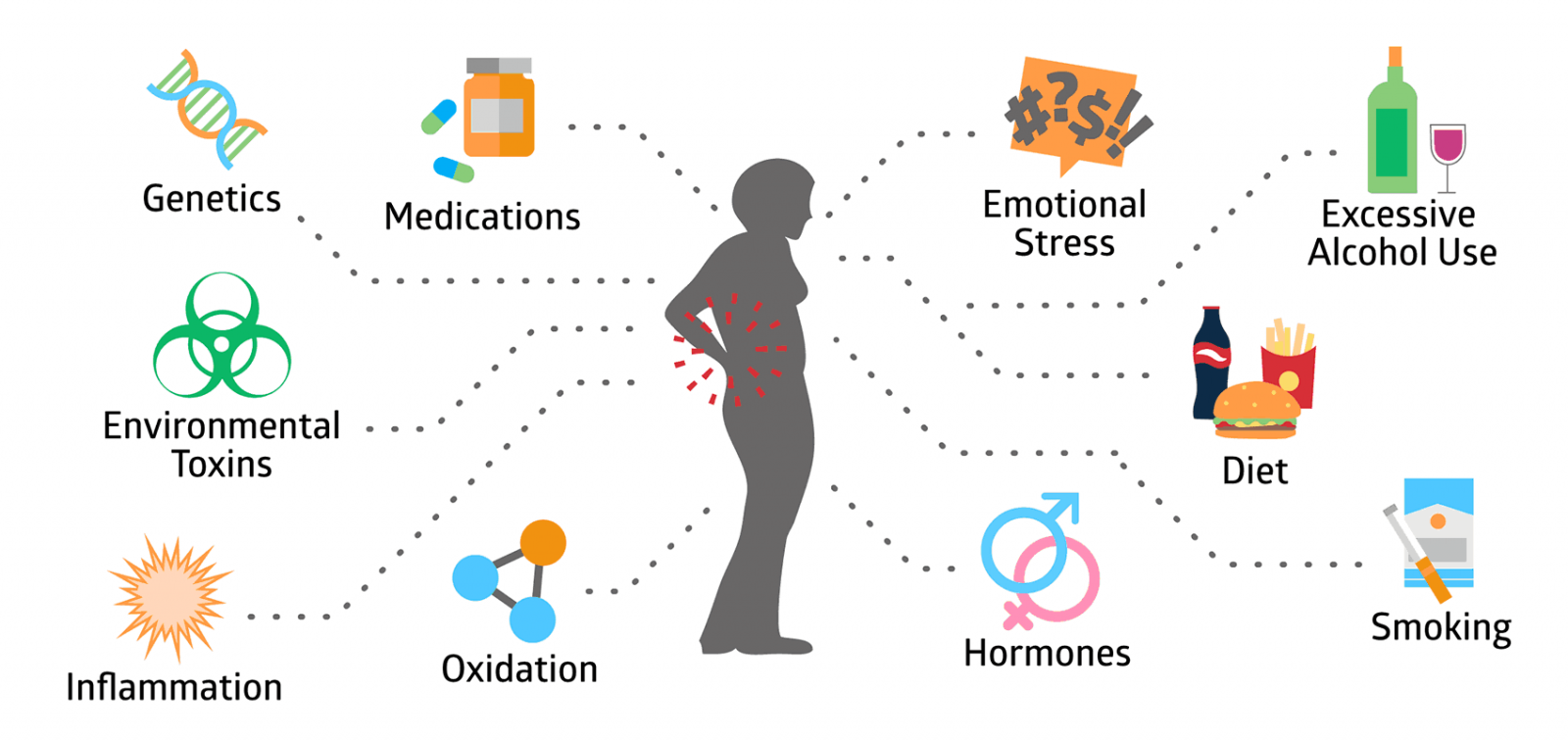
Fractures and their complications are the relevant clinical sequelae of osteoporosis. Osteoporosis is a silent disease until the patient experiences a fracture. A recent fracture at any major skeletal site, such as vertebrae , proximal femur , distal forearm , or shoulder in an adult older than 50 years with or without trauma, should suggest that the diagnosis of osteoporosis needs further urgent assessment involving diagnosis and treatment. Clinical risk factors are listed in . The pathogenesis of osteoporosis-related fractures is summarized in .
Pathogenesis of osteoporosis-related fractures
Low Bmd Predicts Increased All
summarizes reported associations between BMD and all-cause and CVD mortality in ESRD. Compared with the general population where there is an abundance of data, the relationship between BMD and CVD mortality in ESRD is less clear due to the relatively small number of patients and publications in this field. Most previous reports regarding ESRD patients analysed the association between BMD and all-cause mortality, while only a few studies investigated the relationship between BMD and CVD mortality in ESRD patients .
In the study by Taal et al. , reduced total hip BMD measured by central DXA was significantly associated with poor outcomes after adjusting for age, calcium × phosphorus product and previous allograft, whereas there was no significant association between reduced spine BMD and clinical outcome. In line with this, another study reported similar results after adjusting for age, Davies score, dyslipidaemia, albumin and CAC score . Furthermore, another study reported that forearm sites in addition to femoral neck were associated with high all-cause mortality in univariate analysis . Yap et al. used pQCT in addition to DXA in a prospective study of 58 dialysis patients with 6years follow-up and found that tibia cortical density by pQCT, in addition to BMD at femoral neck measured by DXA, was significantly associated with increased all-cause mortality.
Bone mass in ESRD patients is associated with all-cause mortality and CVD mortality.
Epidemiology And Costs Of Ckd
Data from the National Health and Nutrition Examination Survey suggest that CKD and osteoporosis are highly coprevalent . Among NHANES III participants, osteoporosis was twice as common in those with an eGFR<60 ml/min compared with those with an eGFR>60 ml/min . Among women and men with osteoporosis, >80% and 50%, respectively, had a CockcroftGault creatinine clearance <35 ml/min . In patients with predialysis CKD, a history of osteoporosis was reported to be associated with a greater than twofold odds of hip fracture compared with the general population . In general, fractures were reported to be greater than two- to 100-fold more common than in age-matched individuals without CKD , and mortality rates after fracture were greater than threefold greater for patients with than without CKD. In 2010, health careassociated costs after fracture for patients with CKD exceeded $600 million . Thus, there is urgency for nephrologists to treat CKD-associated osteoporosis.
The Link Between Inflammatory Bowel Disease And Osteoporosis
People with IBD are often treated with medications known as glucocorticoids to reduce the inflammation caused by their disease. Over time, these drugs interfere with the development and maintenance of healthy bones. Bone loss increases with the amount and length of glucocorticoid therapy.
In addition, people with severe inflammation of the small bowel or those who have parts of the small bowel surgically removed may have difficulty absorbing calcium and vitamin D. This is an additional concern for bone health.
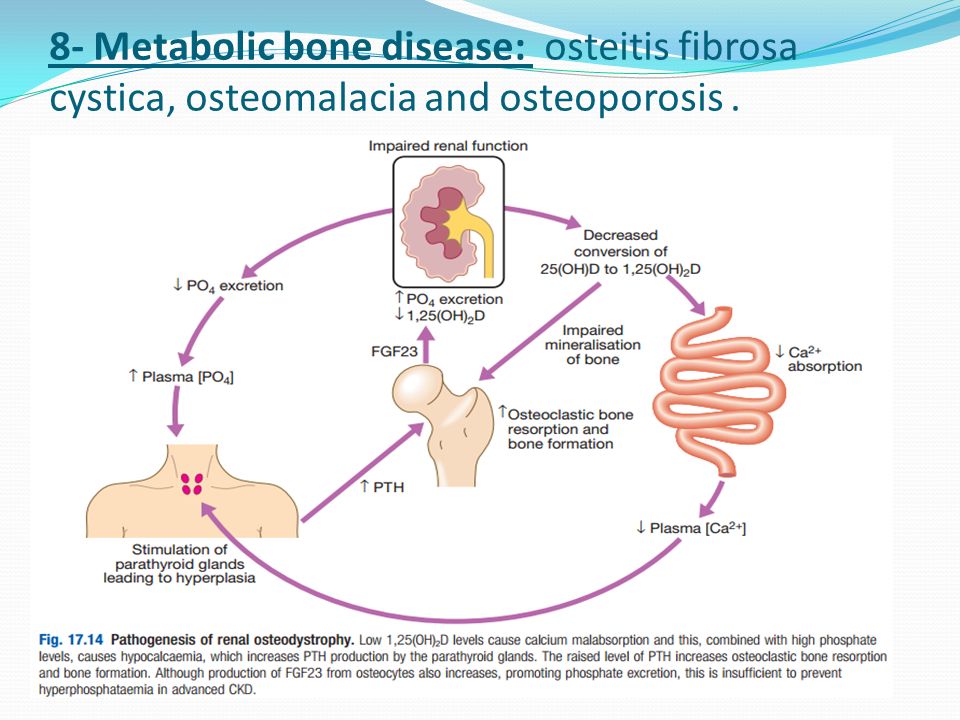
How Is Mineral And Bone Disorder In Chronic Kidney Disease Treated
Treating mineral and bone disorder in CKD includes preventing damage to bones by controlling parathyroid hormone levels through changes in eating, diet, and nutrition; medications and supplements; and dialysis. If these treatments do not bring parathyroid hormone levels under control, a health care provider may remove a persons parathyroid glands surgically, a procedure called a parathyroidectomy.
How Does Eating Diet And Nutrition Affect Anemia In Ckd
You may need to change what you eat to manage your anemia and CKD. Work with your health care professional or a registered dietitian;to develop a meal plan that includes foods that you enjoy eating while maintaining your kidney health and managing your anemia.
If your body doesnt have enough iron, vitamin B12, or folate, your health care professional or a dietitian may suggest that you add more foods with these nutrients to your diet. However, some of these foods have high amounts of protein, sodium, or phosphorus, which people with CKD may need to limit. Talk with your health care professional or a dietitian before making any changes to your diet.
Biochemical Bone Turnover Marker
Bone remodeling occurs throughout life to repair fatigue damage and microfractures in the bone and to maintain mineral homeostasis. Biochemical markers of bone remodeling include resorption markers, namely serum C-terminal telopeptide type-I collagen and urinary N-telopeptide , and formation markers, such as serum procollagen type-I N-terminal propeptide , which may provide information on fracture risk independent of BMD and predict the rapidity of bone loss in untreated patients. Therefore, the fracture risk prediction might get enhanced by their inclusion in assessment algorithms. Further, they can be used to predict the response to treatments. It was shown that there is a significant relationship between the reduction in BTMs following antiresorptive therapy and reduction in vertebral and non-vertebral fracture risk. In general, these studies showed that the greater the decrease in BTM, larger is the reduction in fracture risk.
International Osteoporosis Foundation and International Federation of Clinical Chemistry and Laboratory Medicine Working Group evaluated BTMs in the prediction of fracture risk and for monitoring treatment; it was recommended that bone formation markers and bone resorption markers should be used as reference markers and measured by standardized assays in observational and intervention studies .
Following studies are necessary to rule out secondary osteoporosis :
Serum protein electrophoresis , serum immunofixation, and serum-free light chains
Osteoporosis And Fracture Risk In Patients With Ckd And Renal Replacement Therapy
It is well known that patients with CKD stages 3a-5D have increased fracture rates compared to the general population . A prospective study on 10,955 participants from the atherosclerosis risk in communities study demonstrated a higher risk for fracture if the estimated GFR was below 60;ml/min/1.73;m2 . A retrospective analysis of 2096 patients on renal replacement therapy showed that the symptomatic fracture risk in the renal replacement therapy population appeared to be twice as high in hemodialysis patients as in renal transplantation patients, while peritoneal dialysis patients had an intermediate risk . The consequences of fractures may be more severe in CKD patients. Hospital stay duration in patients with hip fractures was 7;days in patients with end-stage renal disease compared to 5;days in patients without CKD, and the mortality was 5.9% in ESRD, 3.7% in CKD and 1.6% in patients with normal renal function .
Who Should Be Considered For Treatment
Postmenopausal women and men aged 50 years and above who present with the following should be considered for treatment:
-
– A hip or vertebral fracture because it was shown that the patients with spine and hip fractures had reduced fracture risk with pharmacologic therapy, irrespective of the T score.
-
– Determination of fractures when the T-score 2.5 at the femoral neck, total hip, or lumbar spine
-
– Low bone mass and
-
– 10-year probability of a hip fracture 3% or a 10-year probability of a major osteoporosis-related fracture 20%
The anti-fracture benefits of Food and Drug Administration -approved drugs have mostly been studied in women with postmenopausal osteoporosis. There are limited fracture data for men and cases involving glucocorticoid-induced osteoporosis.
What Causes Anemia In Ckd
Anemia in people with CKD often has more than one cause.
When your kidneys are damaged, they produce less erythropoietin , a hormone;that signals your bone marrowthe spongy tissue inside most of your bonesto make red blood cells. With less EPO, your body makes fewer red blood cells, and less oxygen is delivered to your organs and tissues.
In addition to your body making fewer red blood cells, the red blood cells of people with anemia and CKD tend to live in the bloodstream for a shorter time than normal, causing the blood cells to die faster than they can be replaced.
People with anemia and CKD may have low levels of nutrients, such as iron, vitamin B12, and folate, that are needed to make healthy red blood cells.
Other causes of anemia related to CKD include
- blood loss, particularly if you are treated with dialysis;for kidney failure
- infection
- examine your body, including checking for changes in skin color, rashes, or bruising
Family And Medical History
Taking a medical and family history is one of the first things a health care provider may do to help diagnose mineral and bone disorder in CKD. He or she will ask the patient or caretaker questions about when the patient was first diagnosed with CKD and whether any family members have also had mineral and bone disorder with or without CKD.
Pharmacological Treatments For Osteoporosis In Patients With Chronic Kidney Disease
What is the issue? Patients with chronic kidney disease have an increased risk of osteoporosis , which can often lead to bone fracture. Several drugs are available for the treatment of osteoporosis; however, it is unknown whether these drugs are equally effective and safe in patients with CKD because bone strength impairment in these patients occurs via a different mechanism.
What did we do? Data were collected from studies including patients with osteoporosis and CKD stages 3-5, and those undergoing dialysis with data available on fracture, change in the bone mineral density , and adverse events. We included seven studies with available evidence up to 25 January 2021, comparing anti-osteoporotic drugs with placebo , in 9,164 postmenopausal women. We performed a meta-analysis to assess the effects of these anti-osteoporotic drugs.
What did we find? In postmenopausal women with CKD stages 3-4, anti-osteoporotic drugs may reduce vertebral fracture in low certainty evidence. Anti-osteoporotic drugs probably make little or no difference to clinical fracture and adverse events in moderate certainty evidence. In postmenopausal with CKD stages 5 or 5D, it is uncertain whether anti-osteoporotic drug reduces the risk of clinical fracture and death, and anti-osteoporotic drug may slightly improve BMD at the lumbar spine in low certainty evidence. It is uncertain whether anti-osteoporotic drug improve BMD at the femoral neck.
How Is Renal Osteodystrophy Diagnosed
To diagnose renal osteodystrophy, your doctor may take a sample of your blood to measure levels of calcium, phosphorus, PTH, and calcitriol. The doctor may perform a bone biopsy to see how dense your bones are. A bone biopsy is done under local anesthesia and involves removing a small sample of bone from the hip and analyzing it under a microscope. Determining the cause of renal osteodystrophy helps the doctor decide on a course of treatment.
How Do I Know If I Have Mineral And Bone Disorder
- You will have blood tests to check your blood levels of calcium, phosphorus, PTH and vitamin D.
- Some people may need to have a bone biopsy. A bone biopsy is a sample of bone taken for study.
- Your healthcare provider may order an x-ray of your abdomen, or an echocardiogram of your heart to check if mineral imbalance has affected your heart and blood vessels.