How Is Angiotensin Controlled
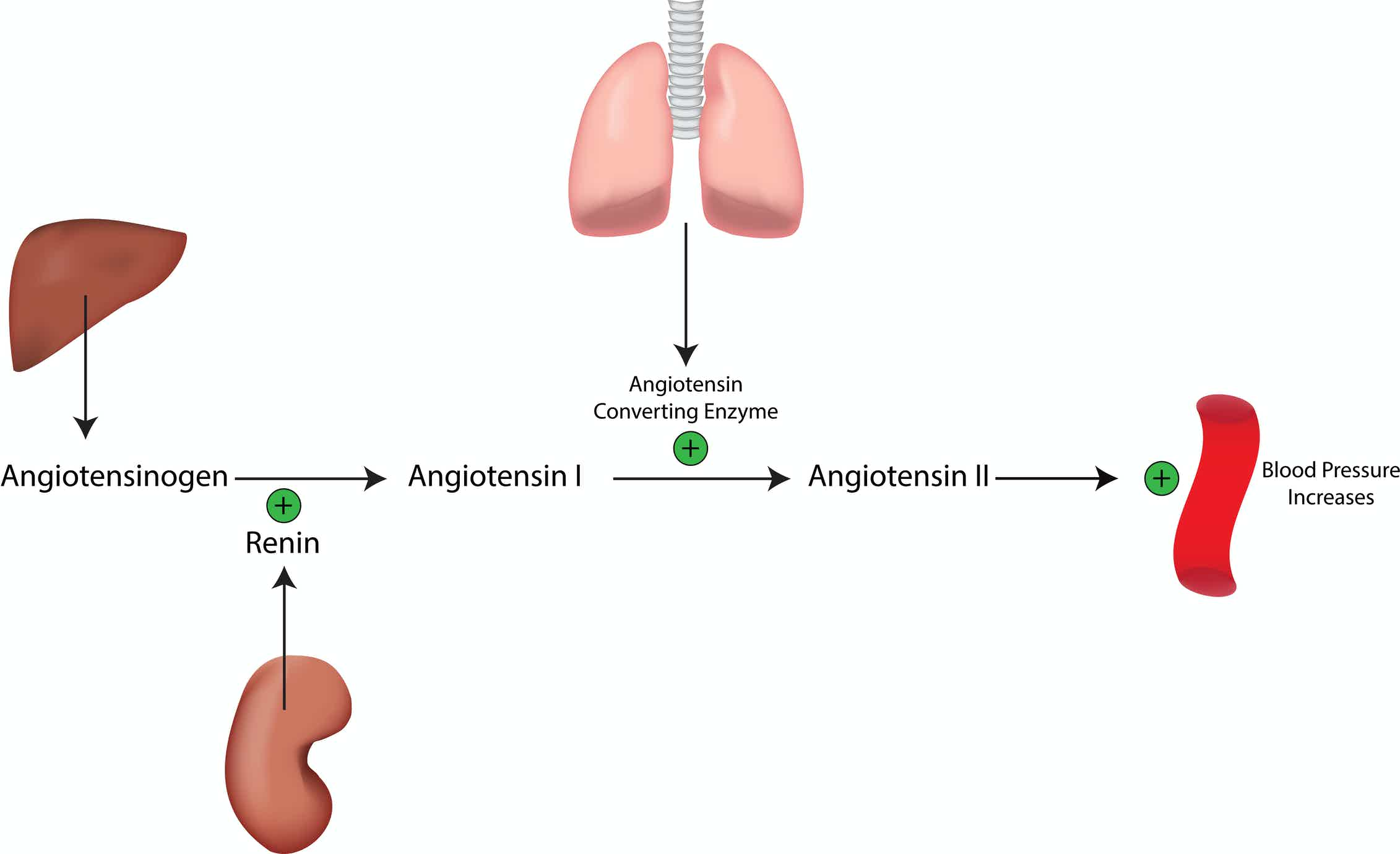
An increase in renin production occurs if there is a decrease in sodium levels and a decrease in blood pressure, which is sensed by the kidneys. In addition, low blood pressure can stimulate the sympathetic nervous system to increase renin production, which results in increased conversion of angiotensinogen to angiotensin I, and so the cycle continues.
The reninangiotensin system is also activated by other hormones, including oestrogen” rel=”nofollow”>oestrogen and thyroid hormones. On the other hand, natriuretic peptides can impede the reninangiotensin system in order to increase sodium loss in the urine.
Elevated Ace In Hemodialysis Patients
In 1979, Patel et al. performed one of the first and best known evaluations of the levels of ACE in HD patients . They studied 19 patients with CKD on long-term HD and 19 controls, and found that ACE activity was increased in 58% of the patients . They proposed that these increased serum ACE levels might be secondary to increased pulmonary vascular area in patients with renal failure, because ACE was thought to be produced only in the lungs. In 1982, Muira et al. confirmed these results but proposed a different mechanism. They noted that the ACE activity of patients with CKD on regular HD was higher than that of age-matched controls , and they also found higher ACE levels in patients on HD for longer than 3 years and in patients with diabetic nephropathy. It is important to note that elevated ACE also occurs in DM . Muira et al. found no relationships of enzyme activity with age and sex . Based on studies reporting accelerated atherosclerosis in patients on maintenance HD, they speculated that advanced endothelial damage could lead to elevated serum ACE in HD patients, because vascular endothelial cells of the lungs and kidneys produce most of the ACE.
Physiological Control Of Renin Secretion In Vivo
The before mentioned findings on the mechanisms controlling renin secretion were mostly obtained in isolated preparations or in laboratory animals under specific conditions that do not provide direct information about the relative contribution of the different pathways to the integrative control of renin secretion in vivo.
The secretion of renin in the normal healthy organism is in the low range, meaning that there is no major regulatory range left to further suppress renin synthesis and renin secretion beyond the normal situation. Conversely, renin synthesis and renin secretion are strongly stimulated if blood pressure, salt homeostasis and/or glomerular filtration are threatened, supporting the notion of an emergency function of the RAAS.
Recommended Reading: Carbonated Water And Kidney Stones
How Does Angiotensin Ii Affect The Kidneys
4.7/5Angiotensin IIeffecteffectrenalAngiotensin II
Similarly one may ask, what are the effects of angiotensin II?
Angiotensin II has effects on: Blood vessels it increases blood pressure by causing constriction of the blood vessels. Nerves: it increases the sensation of thirst, the desire for salt, encourages the release of other hormones that are involved in fluid retention.
Subsequently, question is, how would decreasing the action of angiotensin II reduce blood pressure from a kidney function standpoint? Administration of exogenous Ang II decreases renal blood flow and glomerular filtration rate , and constricts afferent and efferent arterioles dose-dependently11). When the arterial pressure is not obviously reduced, Ang II blockade increases the single nephron GFR as well as the single nephron plasma flow.
Similarly, it is asked, can ARBs cause kidney damage?
Adverse effects Renin-angiotensin system inhibition can be associated with a variety of adverse effects. With respect to progression of the renal disease, ACE inhibitors and ARBs can cause a decline in renal function and a rise in serum potassium that typically occur one to two weeks after the onset of therapy.
What is the effect of angiotensin II on the GFR quizlet?
Genomic Regulation Of Renin Expression
The multiple levels of control for release of renin protein at the JG apparatus are accompanied by a parallel, complex regulation of renin gene expression. The regulatory region of the renin gene has been studied extensively in vitro utilizing a renin expressing cell line isolated from a mouse renal tumor coupled with in vivo studies utilizing transgenic mouse lines. These systems have identified two regions acting in conjunction to control renin expression, including a proximal promoter element and a 242-base pair enhancer region.
Don’t Miss: Can A Kidney Stone Cause Constipation
Processing And Secretion Of Renin In Jg Cells
Renin is initially synthesized as a pre-pro-renin protein. After cleavage of the pre-fragment, pro-renin is transferred to the Golgi. From there, pro-renin can be immediately secreted by the constitutive pathway or sorted to the dense-core secretory granules for regulated exocytosis . It appears that release of pro-renin through the constitutive pathway depends directly on the levels of renin synthesis per se, including levels of transcription per cell and the total number of renin-producing cells . Acute stimulation of renin release involves exocytosis of mature renin secretory granules that contain active renin only whereas chronic stimulation results in release of both pro-renin and renin into the circulation .
Studies in renin knockout mice suggest that glycosylation is crucial for pro-renin sorting into the dense core secretory granules. Ren1 and Ren2 proteins differ in their glycosylation patterns and studies using knock out mice for Ren1 or Ren2 gene show differences in their renin processing. Indeed, deletion of the Ren2 gene alone did not cause an apparent phenotype . In contrast, the kidneys in Ren1 deficient mice showed a very low number or complete absence of dense-core renin vesicles . It has been postulated that glycosylation differences may be responsible for these phenotypic differences .
What Hormones Do The Kidneys Produce
The kidneys make two main hormones, vitamin D and erythropoietin.
Vitamin D is essential for a number of different functions in the body. Most of the vitamin D that is in the blood is inactive and it is modified by the kidney and other tissues to activate it. Active vitamin D stimulates the uptake of calcium from food, is important for the maintenance of healthy bones and also helps to regulate the response of the immune system to infection.
Erythropoietin is produced when oxygen levels in the blood are low. It acts in bone marrow to stimulate the production of mature red blood cells, to maintain healthy oxygen levels in our tissues.
The kidneys also produce prostaglandins, hormone-like substances, made from lipid . The substances are one way in which the production of renin is stimulated. Renin is an enzyme, also produced by the kidneys, that plays an important role in the reninangiotensinaldosterone hormonal system, which helps to control blood pressure. In addition to making hormones, the kidneys also respond to a number of hormones including vitamin D, aldosterone, prostaglandins, cortisol, parathyroid hormone and calcitonin.
Also Check: Celery Juice Good For Kidneys
What Causes The Kidneys To Stimulate Renin Production What Is Renin For
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Nacl Reabsorption At The Macula Densa
The second major pathway for physiological regulation of renin is the macula densa mechanism whereby cells at the macula densa sense a reduction in chloride ions in the filtrate of the distal tubule, triggering renin release . In this circumstance, release of renin and the consequent generation of Ang II are believed to serve as a mechanism for enhancing renal sodium reabsorption in states of fluid volume depletion. The anatomical association of the macula densa with the JG apparatus stimulated the first speculation by Goormaghtigh of its physiological function . The macula densa is made up of specialized epithelial cells at the terminal portion of the thick ascending limb. Their basolateral membrane is in contact with glomerular mesangial cells, which, in turn, are contiguous with granular cells in the JG apparatus . The role of the macula densa in renin regulation was initially hypothesized by Vander in 1967 and there is now general consensus that this mechanism provides a control of renin secretion that is directly determined by NaCl delivery to the distal nephron . Moreover, several studies indicate that chloride flux through the NKCC2 regulates the signaling pathways linked to renin secretion . Increased chloride delivery to the macula densa inhibits, whereas reduced chloride delivery stimulates renin release .
You May Like: Constipation Or Kidney Stone
How The Alternative Ras Pathway Works
Eventually, angiotensin I, angiotensin II, and aldosterone are broken down into other molecules. Some of these other molecules act in a closely related alternative pathway that counteracts the effects of the classical pathway. Important members of the alternative pathway include:
- Angiotensin-converting enzyme 2
- Angiotensin-
- Angiotensin-
While the classical RAS pathway controls blood pressure and body fluid, it also has a complementary negative effect on the body that promotes inflammation. Some of the inflammatory responses of the classical RAS pathway include:
- Blood vessel narrowing, or constriction
- Increase in lung inflammatory responses
- Increase in cell stress responses
- Increase in arrhythmias or abnormal heartbeats
- Increase in insulin resistance
The alternative RAS pathway opposes the effects of angiotensin II by lowering blood pressure. It also has anti-inflammatory responses. Some of these responses include:
- Blood vessel relaxation, or dilation
- Maintains blood flow and oxygenation in the lung
- Reduction in cell stress responses
- Relaxation of the hearts coronary vessels
You can think of the alternative RAS system as a brake on the classical RAA pathway. Because the classical and alternative RAA pathways oppose one another, they act to balance out their systemic effects.
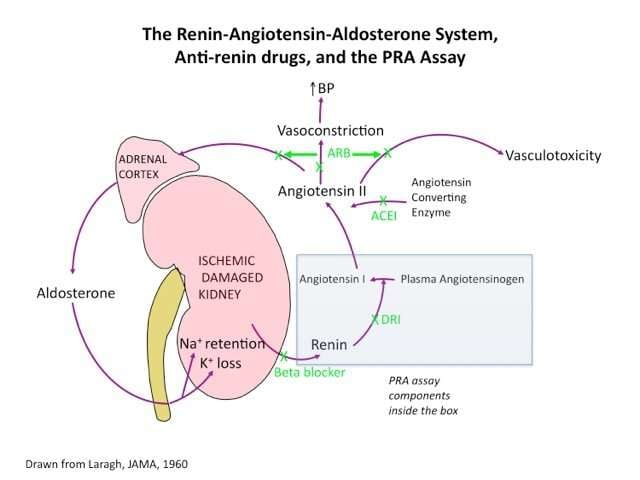
Indirect Tubular Effects Of Ang Ii On Sodium Reabsorption Via Aldosterone
ANG II is a very powerful regulator of aldosterone release by the adrenal gland. The increased aldosterone levels synergize with the direct tubular effects of ANG II to enhance distal tubule sodium reabsorption. Aldosterone increases sodium reabsorption in the distal segments of the nephron by binding to the cytoplasmic mineralocorticoid receptor. On binding, the receptor complex migrates to the nucleus, where it induces gene transcription. Expression of proteins that stimulate sodium reabsorption is enhanced by the increased expression of proteins that stimulate sodium reabsorption by the following mechanisms:
Increasing sodium-potassium ATPase protein and activity at basolateral membranes of distal nephron segments.
Increasing the activity of enzymes of the tricarboxylic acid cycle.
Increasing the production of ATP to be used as an energy source for the sodium-potassium ATPase pump.
Increasing the expression and activation of epithelial sodium channels, which enhances sodium entry into the cell.
Increasing the permeability of the apical membrane to potassium, which drives the ATPase pump.
Taken together, the activation of multiple sodium transport mechanisms leads to augmented sodium and water reabsorption by the kidney.
Recommended Reading: Almond Milk Good For Kidneys
The Raa System And Covid
The Coronavirus disease 2019 , or SARS-CoV-2, led to a global outbreak that affected nearly 200 million people worldwide as of July 2021. The disease is associated with severe complications in people who have pre-existing cardiovascular diseases, such as hypertension and diabetes.
The renin-angiotensin system plays an important role in the COVID-19 infectious disease process.
The SARS-CoV-2 uses angiotensin-converting enzyme 2 as a “receptor” and cellular entry point to infect a wide range of cells in the body. More specifically, ACE 2, which is embedded in the surfaces of cells, is recognized by spike proteins on the COVID-19 virus. This recognition leads to a lock-and-key relationship that opens the door for the virus to enter.
How Is Protein Digested In Our Body
Once a protein source reaches your stomach, hydrochloric acid and enzymes called proteases break it down into smaller chains of amino acids. Amino acids are joined together by peptides, which are broken by proteases. From your stomach, these smaller chains of amino acids move into your small intestine.
Recommended Reading: Celery Juice Kidneys
Role Of The Ras In Response To Changes In Effective Circulating Volume
Fig. 3.Regulatory responses to ECF volume contraction. The integrated response of the nephron to ECF volume contraction results in the following: decreased glomerular filtration rate , increased NaCl and water reabsorption by the proximal tubule and loop of Henle , and increased NaCl and water reabsorption by the distal tubule and collecting duct . ANP, atrial natriuretic peptide BNP, brain natriuretic peptide ADH, antidiuretic hormone.
The integrated response of the nephron to volume contraction results in the following: 1) decreased GFR, 2) increased sodium chloride and water reabsorption by the proximal tubule and loop of Henle, and 3) increased sodium chloride and water reabsorption by the distal tubule and collecting duct. The RAS is integrally involved in regulating GFR and enhancing sodium chloride and water reabsorption in proximal and distal nephron segments. The final outcome is a reduction in salt and water excretion and preservation of ECF volume and blood pressure.
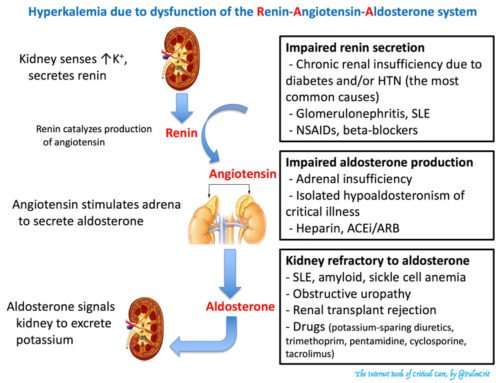
Effects Of Ang Ii On Potassium Secretion
Increases in plasma potassium concentration directly increase the release of aldosterone from the adrenal cortex, independent of the actions of ANG II. Aldosterone increases potassium secretion in the distal segments of the nephron. Aldosterone stimulates potassium secretion by increasing the following:
Sodium-potassium ATPase protein and activity at the basolateral membrane of distal nephron segments, which increases the electrochemical driving force for potassium entry into the cell and increases the secretion of potassium across the apical membrane.
Activity of enzymes of the tricarboxylic acid cycle.
Production of ATP to be used as an energy source for the sodium-potassium ATPase pump.
The expression and activation of epithelial sodium channels, which enhances sodium entry into the cell and increases lumen negativity, which then increases the secretion of potassium.
Permeability of the apical membrane to potassium by increasing the number of potassium channels and enhancing the activation of these potassium channels.
Therefore, increasing apical secretion of potassium increases potassium excretion by the kidneys.
Don’t Miss: Can A Kidney Infection Cause Diarrhea
Short Loop Feedback: Regulation Of Renin By Ang Ii
AT1 receptors are also highly expressed in the JG apparatus and Ang II may exert an inhibition of renin release by the short-loop feedback mechanism. Treatment with RAS antagonists or genetic ablation of the AT1A receptor in mice increases renin mRNA expression and causes JG apparatus expansion with recruitment renin-containing cells . In addition, infusion of Ang II into isolated perfused kidneys inhibits renin release . AT1 receptors couple to Gq proteins and activation of these receptors by ligand increases intracellular Ca2+ concentrations in JG cells . As discussed above, the inhibitory effect of Ca2+ on renin release appears to be mediated by protein kinase C since stimulation of protein kinase C inhibits renin secretion, whereas blockade of protein kinase C attenuates the inhibitory effect on renin secretion . There is also evidence that the effects of Ca2+ on renin release are mediated in part by a calmodulin-dependent process, since inhibition of calmodulin activity stimulates renin secretion . On the other hand, in kidney cross transplantation experiments with AT1A receptor deficient mice indicated that stimulation of renin expression was more directly associated with reduced blood pressure rather than direct modulation by AT1 receptors .
Raa Inhibitors And High Blood Pressure
Several effective high blood pressure treatments have been developed as a direct result of our understanding of the renin-angiotensin-aldosterone system.
- ACE inhibitors stop the conversion of angiotensin I to angiotensin II.
- Angiotensin receptor blockers prevent angiotensin II from binding to blood vessels and causing vasoconstriction.
- Water pills, or diuretics, help to get rid of fluid by telling the body excrete water and sodium through urination.
While we have a better understanding of how to manage chronic high blood pressure, the fine details of the renin-angiotensin-aldosterone system are still being discovered.
You May Like: Does Carbonated Water Cause Kidney Stones
Sketch Summarizing Processing Of Renin And Regulation Of Renin Release Ang I Angiotensin I Camp Cyclic Adenosine Monophosphate
Sorting of prorenin is either directed to a prominent electron dense vesicular network, or to the constitutive secretory pathway which leads to the direct release of prorenin. Up to 80% of the produced prorenin can be directly released into circulation in men. Circulating prorenin can bind to a specific membrane protein named prorenin receptor. By binding to the receptor prorenin can initiate profibrotic signaling pathways and can also gain some enzymatical activity and cleave angiotensin I from angiotensinogen, a process that is normally restricted to renin. The physiological relevance of those prorenin effects, however, is yet unclear. If and where prorenin can be enzymatically activated in the extracellular space is unknown. Prorenin can be taken up into cells such as in cardiomyocytes where it may be activated to renin.
The Kidneys Are Stimulated To Produce Renin True Or False
True
Explanation:
Kidneys are defined as a pair of bean-shaped organ present in the abdominal cavity of mammals, reptiles, and birds responsible for excretion of urine.
Renin is a peptide hormone which is secreted by the kidneys from granular cells that are present in the juxtaglomerular apparatus. The secretion of renin stimulation is based on decrease in sodium chloride in the juxtaglomerular apparatus by the macula densa, fall in arterial blood pressure in the arterial vessels by baroreceptors and sympathetic nervous system activity is through beta 1 adrenergic receptors.
Hence, the given statement is true.
C) by a decrease in the blood pressure
Read Also: Is Cranberry Juice Good For The Liver
What Happens If I Have Too Little Angiotensin
Control of plasma sodium and potassium concentrations, and the regulation of blood volume and pressure, are all hormonal mechanisms that are impaired by low angiotensin levels. Absence of angiotensin can be associated with retention of potassium, loss of sodium, decreased fluid retention and low blood pressure.
What Is The Connection Between Renin And Blood Pressure
The connection between renin and blood pressure is that the production of renin causes blood pressure to rise. Renin is an enzyme produced by the kidneys. It is a key component of the renin-angiotensin system, a series of processes that raises blood pressure in abnormal situations. The body, for many reasons, can produce too much renin that leads to a state of maintained high blood pressure. This disorder is known as hypertension.
One of the main functions of the kidneys is to maintain proper blood pressure through reabsorbing water and electrolytes, or expelling them as urine. This process is gradual and, in a healthy body at rest, works normally. Yet, if one or a combination of three events occurs, the kidneys need assistance in raising blood pressure quickly. The three triggers are a sudden decrease in blood pressure, a fight or flight response created by the body’s nervous system, and a lack of electrolytes in the blood.
Don’t Miss: Is Grape Juice Good For Kidney Stones