Why Is It Difficult To Raise Urine Sodium Concentration
The difficulty to excrete sodium appears to be due to the limited ability of the kidney to raise UNa when V cannot increase because of the low availability of water. This appears clearly in Figure 4b. After the load, UNa did not increase further in subjects who already exhibited a relatively high UNa before the load, and UNa did not exceed 280 mmol/L in any subject. An interesting observation is provided by a study performed in minks submitted to different salt intakes by adding 0.5, 1, or 2% NaCl to their usual diet for 4 days at each level . The addition of 0.5% NaCl did not modify water intake, whereas the addition of 1 or 2% salt doubled and almost quadrupled the volume of water consumed, respectively. Figure 4c shows that the adaptation to progressively increasing sodium intakes initially was achieved almost exclusively by a marked rise in UNa without much change in V. With a further rise in sodium intake, UNa reached a plateau and sodium excretion increased mostly as a result of a rise in V. These observations in minks and in humans show that the physiological limit to the ability of the kidney to concentrate sodium is about 2-2.5 times the plasma sodium concentration. In contrast, other solutes like potassium, urea, uric acid, ammonia and so on can be concentrated in the urine 10-1,000-fold above their plasma value . Note that these solutes exhibit much lower concentrations in plasma than sodium .
What Hormone Influences Sodium Reabsorption In The Kidney Is
Aldosterone
. In respect to this, what hormones are involved in kidney function?
Endocrine functions of the kidneys. The kidneys produce three important hormones: erythropoietin, calcitriol and renin. They also synthesize prostaglandins, which affect many processes in the kidneys .
Similarly, why is sodium reabsorption so important in the kidney? Substances are reabsorbed from the tubule into the peritubular capillaries. This happens as a result of sodium transport from the lumen into the blood by the Na+/K+ATPase in the basolateral membrane of the epithelial cells. The kidneys sense low blood pressure. Release renin into the blood.
Beside above, what hormones are involved in reabsorption?
Some key regulatory hormones for reabsorption include:
- aldosterone, which stimulates active sodium reabsorption
- antidiuretic hormone, which stimulates passive water reabsorption.
How is sodium regulated by the kidneys?
Regulation of Salt and Water BalanceSodium and water balance are precisely regulated by the endocrine system. Renal mechanisms that govern retention or loss of sodium are regulated by the renin-angiotensin-aldosterone system and the atrial natriuretic factor.
Kidneys Regulate Blood Pressure
Another important function of the kidneys include blood pressure regulation. One of the ways in which kidneys regulate blood pressure is by removing excessive water within the blood thatmay otherwise lead to increased blood pressure. In contrast, if blood pressure is low, kidneys will produce an enzyme called renin to increase it.
An enzymes is a substance that facilitates chemical exchanges within the body. Renin works by starting a series of chemical reactions in the body that play a role in increasing blood pressure. Renin is also required for the production of another chemical called angiotensin I which needs to be changed into angiotensin II before it can serve its function of increasing blood pressure. This is accomplished by an enzyme called angiotensin converting enzyme which turns angiotensin I into angiotensin II. Angiotensin II raises blood pressure by stopping the kidneys from taking salt and water out of the blood and making blood vessels narrower. With more blood having to move through a smaller space the outcome is increased blood pressure.
However, a chronically high blood pressure can damage the blood vessels within the body, particularly the smaller and finer ones, such as the ones found in the kidneys. The damaged kidneys may in turn fail to remove excess water from the body, which may in turn result in higher blood pressure leading to a very dangerous cycle.
Read Also: What Std Messes With Your Kidneys
Inner Medullary Collecting Duct
As assessed by in vivo microcatheterization of the IMCD, rates of Na+ reabsorption were proportional to rates of Na delivery to the segment and modified by infusion of KCl . This phenomenon was not observed in isolated perfused tubules , but in that preparation high flow rates abolish the effect of atrial natriuretic peptide to inhibit absorption.
How Is Glucose Delivered To Cells
The glucose we eat is broken down through glycolysis and used to power the many processes of our cells. Thus, it is essential to supply each of our cells with a steady stream of glucose. Glucose is delivered throughout the body by the blood, and each cell gathers what it needs using glucose transporters.
You May Like: What Laxative Is Safe For Kidneys
Kidneys Produce Important Hormones
The kidneys are also responsible for producing important hormones such as Calcitriol and erythropoietin. Calcitriol is also known as the active form of Vitamin D which has many functions in the body including: immune system enhancement, contribution to bone health, regulation of phosphorus and calcium levels and even cancer prevention.
The hormone erythropoietin also plays an important role as it is responsible for stimulating the production of red blood cells in the bone marrow. Thus, it plays a role in supporting the supply of oxygen to the muscles and to the brain. A lack of this hormone may lead to a condition called anemia which is characterized by chronic fatigue, overall weakness and lack of concentration resulting from a suboptimal level of oxygen in the body.
These are certainly some of the most important functions performed by the kidneys which show how important they are for our overall well being. It would be unfeasible to cover in detail all of the functions and processes performed by the kidneys within one article. However, if you would like to learn even more interesting and detailed facts about kidney function, then we encourage you to watch the videos presented below :
Fluid And Electrolyte Balance
The kidneys are essential for regulating the volume and composition of bodily fluids. This page outlines key regulatory systemsinvolving the kidneys for controlling volume, sodium and potassium concentrations, and the pH of bodily fluids.
A most critical concept for you to understand is how water and sodium regulation are integrated to defend the body against allpossible disturbances in the volume and osmolarity of bodily fluids. Simple examples of such disturbances include dehydration, bloodloss, salt ingestion, and plain water ingestion.
Water balance
Water balance is achieved in the body by ensuring that the amount of water consumed in food and drink equals the amount of water excreted. The consumption side is regulated by behavioral mechanisms, including thirst andsalt cravings. While almost a liter of water per day is lost through the skin, lungs, and feces, the kidneys are the major site ofregulated excretion of water.
One way the the kidneys can directly control the volume of bodily fluids is by the amount of water excreted in the urine. Either thekidneys can conserve water by producing urine that is concentrated relative to plasma, or they can rid the body of excess water byproducing urine that is dilute relative to plasma.
ADH secretion is influenced by several factors :
1. By special receptors in the hypothalamus that are sensitive to increasing plasma osmolarity . These stimulate ADH secretion.
Sodium balance
Recommended Reading: Std That Affects Kidneys
Is Reabsorption Active Or Passive
Reabsorption includes passive diffusion, active transport, and cotransport. Water is mostly reabsorbed by the cotransport of glucose and sodium. Filtrate osmolarity changes drastically throughout the nephron as varying amounts of the components of filtrate are reabsorbed in the different parts of the nephron.
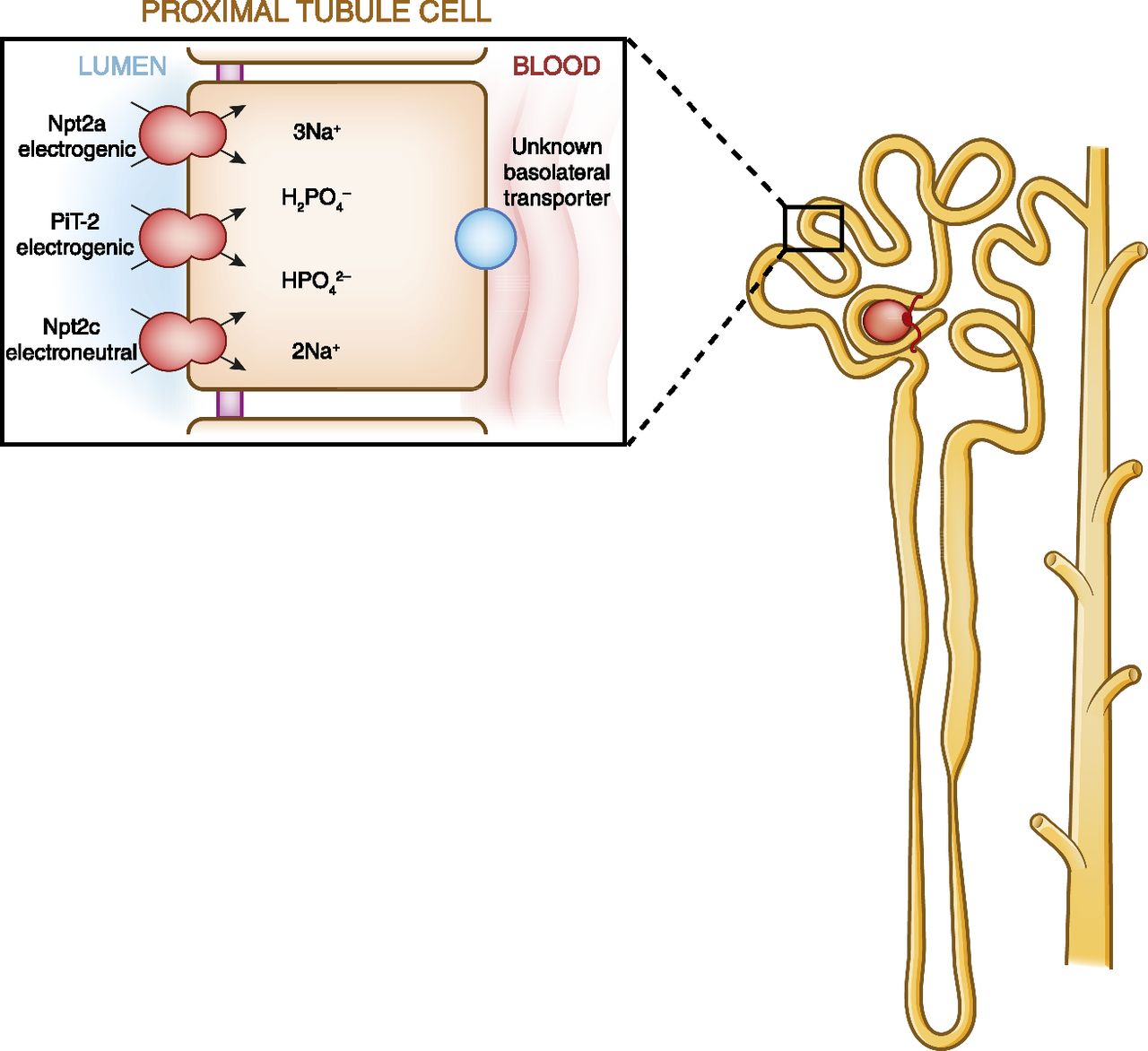
Na Reabsorption Along The Nephron
Micropuncture and microperfusion studies have shown that all nephron segments contribute to the retrieval of filtered Na . The reabsorption of Na is an energy-consuming process that is powered by a Na- and K-activated ATPase in the basolateral membranes of all Na-reabsorbing cells in the kidney. Oxygen consumption of the kidneys is similar to that of other major organs and is extracted from a seemingly excessive blood supply. While the kidneys consume between 7% and 10% of total oxygen uptake, they receive about 20%25% of cardiac output at rest. Two thirds or more of renal oxygen uptake are expended for the needs of the Na,K-ATPase, which is for active Na reabsorption.
Na transport along the nephron. The fraction of Na remaining in the ultrafiltrate is plotted as a function of distance along the nephron under conditions of normal salt intake. The cartoon indicates the major nephron segments. The symbols below show the key Na transport mechanisms in each segment. CCD, cortical collecting duct CNT, connecting tubule DCT, distal convoluted tubule IMCD, inner medullary collecting duct OMCD, outer medullar collecting duct PCT, proximal convoluted tubule PST, proximal straight tubule S, solute tAL, thin ascending limb TAL, thick ascending limb tDL, thin descending limb.
Don’t Miss: Can You Have 4 Kidneys
Why Does The Body Reabsorb Glucose In Kidney Filtration
Renal glucose reabsorption is the part of kidney physiology that deals with the retrieval of filtered glucose, preventing it from disappearing from the body through the urine. Once in the tubule wall, the glucose and amino acids diffuse directly into the blood capillaries along a concentration gradient.
Gitelman And Bartter Syndromes
Our understanding of renal sodium reabsorption and potassium excretion is, in part, a result of intense efforts to identify families with blood pressure and serum potassium levels that markedly deviate from the population means. Several of these traits have shown patterns consistent with classic Mendelian transmission within families, enabling genetic mapping and gene identification. Gitelman and Bartter syndromes, discussed in detail elsewhere in this volume, are excellent examples which have proved instructive for understanding magnesium homeostasis .
Peter A. Doris, in, 2007
Read Also: Is Celery Juice Good For Kidneys
Reabsorption And Secretion In The Distal Convoluted Tubule
Approximately 80 percent of filtered water has been recovered by the time the dilute forming urine enters the DCT. The DCT will recover another 10â15 percent before the forming urine enters the collecting ducts. Aldosterone increases the amount of Na+/K+ ATPase in the basal membrane of the DCT and collecting duct. The movement of Na+ out of the lumen of the collecting duct creates a negative charge that promotes the movement of Clâ out of the lumen into the interstitial space by a paracellular route across tight junctions. Peritubular capillaries receive the solutes and water, returning them to the circulation.
Cells of the DCT also recover Ca++ from the filtrate. Receptors for parathyroid hormone are found in DCT cells and when bound to PTH, induce the insertion of calcium channels on their luminal surface. The channels enhance Ca++ recovery from the forming urine. In addition, as Na+ is pumped out of the cell, the resulting electrochemical gradient attracts Ca++ into the cell. Finally, calcitriol is very important for calcium recovery. It induces the production of calcium-binding proteins that transport Ca++ into the cell. These binding proteins are also important for the movement of calcium inside the cell and aid in exocytosis of calcium across the basolateral membrane. Any Ca++ not reabsorbed at this point is lost in the urine.
What Is The Responsibility Of The Sodium
It acts to transport sodium and potassium ions across the cell membrane in a ratio of 3 sodium ions out for every 2 potassium ions brought in. In the process, the pump helps to stabilize membrane potential, and thus is essential in creating the conditions necessary for the firing of action potentials.
You May Like: Std And Kidney Pain
Reabsorption And Secretion In The Pct
Figure 2. Substances Reabsorbed and Secreted by the PCT
More substances move across the membranes of the PCT than any other portion of the nephron. Many of these substances use symport mechanisms for transport along with Na+. Antiport, active transport, diffusion, and facilitated diffusion are additional mechanisms by which substances are moved from one side of a membrane to the other. Recall that cells have two surfaces: apical and basal. The apical surface is the one facing the lumen or open space of a cavity or tube, in this case, the inside of the PCT. The basal surface of the cell faces the connective tissue base to which the cell attaches or the cell membrane closer to the basement membrane if there is a stratified layer of cells. In the PCT, there is a single layer of simple cuboidal endothelial cells against the basement membrane. The numbers and particular types of pumps and channels vary between the apical and basilar surfaces. A few of the substances that are transported with Na+ on the apical membrane include Clâ, Ca++, amino acids, glucose, and }_^ . Sodium is actively exchanged for K+ using ATP on the basal membrane. Most of the substances transported by a symport mechanism on the apical membrane are transported by facilitated diffusion on the basal membrane. At least three ions, K+, Ca++, and Mg++, diffuse laterally between adjacent cell membranes .
| Table 3. Reabsorption of Major Solutes by the PCT |
|---|
| Basal membrane |
| Ca++ |
| Mg++ |
HCO3â+ H+âH2CO3âCO2H2O
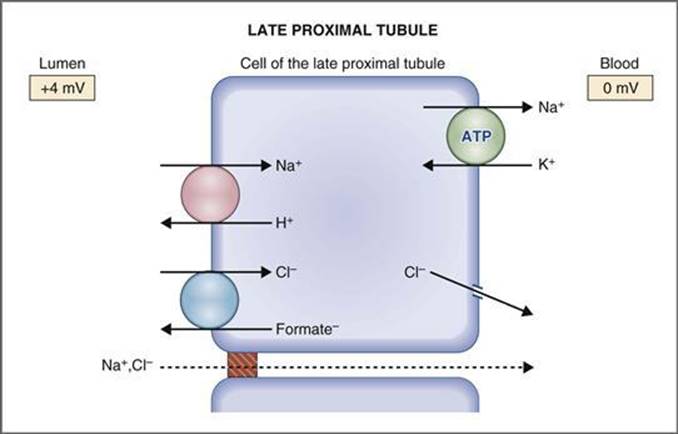
Flow Dependence Of Na Transport
A basic form of communication between parts of the nephron is through changes in Na delivery that result from changes in GFR for the proximal tubule, and from changes in reabsorption in an upstream segment in all other parts of the nephron. In general, a change in delivery provokes a change in downstream absorption in the same direction, thereby blunting the effect of changes in Na input on the output to the downstream segment.
Also Check: Ginger Tea Dissolves Kidney Stones
Is Nacl Passive Or Active
It is concluded that: when PCT lumen are perfused with high chloride solution and the peritubular capillaries perfused with an ultrafiltrate-like solution, approximately 50% of NaCl and water absorption is passive, driven by the anion gradients, and 50% is active when PCT lumen and peritubular capillaries are
Hyperglycemia Assay And Vegf Elisa
In hyperglycemia experiments, the 3D VasPT samples used are 10 d postconfluency. For control samples, the glucose level of cell media remains unchanged. For the hyperglycemia and hyperglycemia with dapagliflozin administration conditions, the glucose level in the PT channel is increased to 400 mg/dL by adding additional d-glucose to the PTEC media. The administered dapagliflozin concentration is 0.5 M. After 48 h of perfusion, CellRox 5 M is perfused through all samples for 30 min. Subsequently, all samples are quickly washed with fresh and warm media and immediately imaged using a confocal microscope.
The level of VEGF-A in the EGM2 is measured using the human VEGF-A ELISA kit per the manufacturers protocol. The VEGF uptake amount is determined by subtracting the VEGF concentration in the perfused media from the initial value of unused EGM2.
Also Check: Seltzer Water And Kidney Stones
Immunostaining Direct Staining And Light Microscopy
Immunostaining followed by confocal microscopy is used to characterize the cellular morphology and localization of proteins. Each tissue is fixed for 30 min to 1 h using 10% buffered formalin . Samples are washed three times in PBS and blocked overnight using a solution of 2% donkey serum and 1 wt % BSA in PBS. Three-dimensional kidney tissues are then incubated with primary antibodies for 1 d at the dilutions listed in SI Appendix, Table S1 in permeabilization buffer . The unbound primary antibodies are then removed from the samples by washing them three times in PBS. Samples were then incubated with secondary antibodies using the dilutions listed in SI Appendix, Table S1 in a solution of 0.5 wt % BSA and 0.125 wt % Triton X-100 in PBS. Finally, the cells are counterstained with NucBlue and ActinRed for 30 min and then washed for several hours in PBS before imaging. For the hyperglycemia assay, CellROX is used to detect the oxidative stress in live GMECs, and nitrogyrosine antibody is used for further confirmation. Bright-field microscopy is performed using a Nikon Eclipse Ts2 scope equipped with a Zeiss AxioCam MRc 5. Confocal microscopy is performed using an upright Zeiss LSM 710 with water-immersion objectives ranging from 5× to 40×. Image reconstructions of z-stacks are performed in ImageJ or IMARIS.
Sodium Handling In The Thick Ascending Limb
The thick ascending limb is impermeable to water, and its apical membrane bristles with frusemide-sensitive NKCC2 Na+ K+ and Cl- co-transporter proteins. Approximately 20-30% of filtered sodium is reabsorbed here. The gradient for the movement of sodium here is again supplied by the basolateral Na+/K+ ATPase which helps suck sodium along its transcellular path.
A second paracellular mechanism plays a role, where a potential difference is generated across the tubule epithelium, driving the sodium across the tight junctions. This electrical gradient is generated by the constant recycling of potassium. Consider: the concentration of potassium in the tubule is always going to be lower than the sodium, which means it can never stay co-transported – after it makes its way into the cell via the NKCC2 channel, it needs to return to the lumen so it can be transported again. This recycling leads to a net buildup of positive charge in the lumen . According to a diagram in Reeves et al , the magnitude of this potential difference is about 10 mV (i.. the tubule lumen is about 10 mV positive as compared to the surrounding interstitium.
Because of the vigorous transport of solutes and minimal transport of water, the thick ascending limb is able to dilute the tubular fluid to the point where its osmolality ends up being close to 90-100 mOsm/kg, with perhaps 25-40 mmol/L of sodium.
You May Like: Is Club Soda Good For Kidney Stones
Target Cells/tissues And Functions
Ang II/AT1 axis mediates vasoconstriction, thirst, release of vasopressin and aldosterone, renal sodium reabsorption, fibrosis, inflammation, angiogenesis, vascular aging, and atherosclerosis. Ang II-induced effects included blood pressure control, increased drinking, adrenergic stimulation, modulation of ion pump and transporter activities in the gill, kidney, and intestine in fish, control of filtering nephron population in fish, and regulation of ventral skin absorption in amphibians . Injection of Ang II significantly increases ventral skin drinking in the frog. Lamprey Ang II is a vasodepressor instead of a vasopressor when injected intra-arterially . Intracerebroventricular injection of Ang II into trout increases systemic blood pressure, heart rate, and ventilation rate. ICV injection of Ang II elicits tachycardia in contrast to bradycardia when injected peripherally. Central Ang II injection also inhibits the vagal-mediated baro-reflex, indicating brain RAS is involved in heart-rate control . The AT2 receptor is mostly embryonic and expression is decreased in adults and is confined in certain tissues such as kidney. The effects of AT2 are often antagonistic to AT1, and activation of AT2 receptors usually indicates a pathophysiological condition of AT1-mediated action with potential harmful consequences. AT2 is abundantly expressed in the spleen of adult eel, which suggested an immune-related function .
H. Sobamowo, S.S. Prabhakar, in, 2017