Acute Kidney Injury Network Classification System
The Acute Kidney Injury Network has developed specific criteria for the diagnosis of AKI. The AKIN defines AKI as abrupt reduction of kidney function, manifested by any 1 of the following :
- An absolute increase in serum creatinine of 0.3 mg/dL or greater
- A percentage increase in serum creatinine of 50% or greater
- A reduction in urine output, defined as less than 0.5 mL/kg/h for more than 6 hours
AKIN has proposed a staging system for AKI that is modified from RIFLE. In this system, either serum creatinine or urine output criteria can be used to determine stage. See Table 2, below.
Table 2. Acute Kidney Injury Network Classification/Staging System for AKI
|
Stage |
||
|
Increase of 0.3 mg/dL or 1.5- to 2-fold increase from baseline |
< 0.5 mL/kg/h for > 6 h |
|
|
> 2-fold to 3-fold increase from baseline |
< 0.5 mL/kg/h for > 12 h |
|
|
> 3-fold increase from baseline, or increase of 4.0 mg/dL with an acute increase of at least 0.5 mg/dL |
< 0.3 mL/kg/h for 24 h or anuria for 12 h |
|
|
*Patients who receive renal replacement therapy are considered to have met the criteria for stage 3 irrespective of the stage they are in at the time of RRT. |
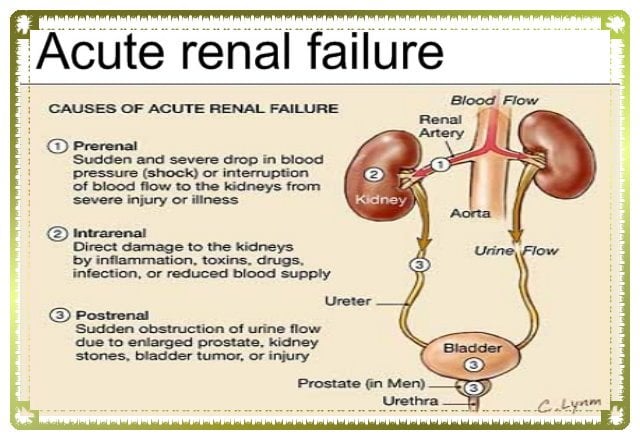
What Are The Causes Of Acute Kidney Disease
Acute kidney disease happens when the kidney suddenly loses its function. The destruction of the kidney function is caused by conditions such as:
Loss of blood flow to the kidneys: Your kidneys need continual blood flow for sifting waste, in the absence of which, the kidneys in the worst scenario may fail ultimately.
Such situations include:
- Continuous internal or external bleeding
- Severe diarrhea
- Using NSAIDs such as aspirin, or ibuprofen
- Serious burns
- Drinking not enough water for a time
- Severe allergic reaction
Direct damage to the kidneys: A few of the situations can impact your kidneys in the first place
- Blood lumps in or around the kidneys
- Diseases that affect the kidneys, such as glomerulonephritis and lupus
- Certain medicines, such as some chemotherapy drugs, antibiotics and contrast dyes used during CT scans, and other imaging tests
- Alcohol or drug misuse
- Some blood or blood vessel disorders
- Hemolytic uremic syndrome
- Idiopathic thrombocytopenic thrombotic purpura
- Malignant hypertension
- Transfusion reaction
- Scleroderma
Occlusion of the urinary tract: Some situations also result in urinary tract obstruction resulting in acute kidney disease.
- Some cancers
- Blood clots in or around the kidneys
- Kidney stones
- Bladder problems
- Enlarged prostate
The diagnosis of Acute Kidney Disease increases if you are an older person with the following risk factors:
- Kidney disease
- Diabetes, especially if its not well controlled
- Morbid obesity
Restoration Of Renal Blood Flow And Associated Complications
Recovery from AKI is first dependent upon restoration of RBF. Early RBF normalization predicts better prognosis for recovery of renal function. In prerenal failure, restoration of circulating blood volume is usually sufficient. Rapid relief of urinary obstruction in postrenal failure results in a prompt decrease of vasoconstriction. With intrinsic renal failure, removal of tubular toxins and initiation of therapy for glomerular diseases decreases renal afferent vasoconstriction.
Once RBF is restored, the remaining functional nephrons increase their filtration and eventually undergo hypertrophy. GFR recovery depends on the size of this remnant nephron pool. If the number of remaining nephrons is below a critical threshold, continued hyperfiltration results in progressive glomerular sclerosis, eventually leading to increased nephron loss.
A vicious cycle ensues continued nephron loss causes more hyperfiltration until complete renal failure results. This has been termed the hyperfiltration theory of renal failure and explains the scenario in which progressive renal failure is frequently observed after apparent recovery from AKI.
Recommended Reading: Kidney Stones Chocolate
What Is The Treatment For Acute Kidney Failure
Your treatment will depend on the cause of your acute kidney failure. The goal is to restore normal kidney function. Preventing fluids and wastes from building up in your body while your kidneys recover is important. In the majority of cases, a kidney specialist called a nephrologist makes an evaluation.
What Is Acute Kidney Injury
Acute kidney injury , also known as acute renal failure , is a sudden episode of kidney failure or kidney damage that happens within a few hours or a few days. AKI causes a build-up of waste products in your blood and makes it hard for your kidneys to keep the right balance of fluid in your body. AKI can also affect other organs such as the brain, heart, and lungs. Acute kidney injury is common in patients who are in the hospital, in intensive care units, and especially in older adults.
Recommended Reading: Kidney Stones And Constipation
Depressed Renal Blood Flow
Depressed RBF eventually leads to ischemia and cell death. This may happen before frank systemic hypotension is present and is referred to as normotensive ischemic AKI. The initial ischemic insult triggers a cascade of events, including production of oxygen free radicals, cytokines and enzymes endothelial activation and leukocyte adhesion activation of coagulation and initiation of apoptosis. These events continue to cause cell injury even after restoration of RBF.
Tubular cellular damage results in disruption of tight junctions between cells, allowing back leak of glomerular filtrate and further depressing effective GFR. In addition, dying cells slough off into the tubules, forming obstructing casts, which further decrease GFR and lead to oliguria.
During this period of depressed RBF, the kidneys are particularly vulnerable to further insults this is when iatrogenic renal injury is most common. The following are common combinations:
-
Radiocontrast agents, aminoglycosides, or cardiovascular surgery with preexisting renal disease
-
Angiotensin-converting enzyme inhibitors with diuretics, small- or large-vessel renal arterial disease
-
NSAIDs with chronic heart failure, hypertension, or renal artery stenosis
C Criteria For Diagnosing Each Diagnosis In The Method Above
The RIFLE criteria should be applied to a patient with suspected of acute renal failure to determine the degree of acute kidney injury and whether or not the patient is oliguric or not. The next step should be take a good history and determine if the patient is at risk for potential causes of pre-renal failure and if their physical exam supports one of these potential diagnosis. If the history and physical are suggestive of one of the low circulating volume states, empiric treatment with volume repletion can be initiated without further diagnostic tests.
Also Check: Is Red Wine Good For Kidney Stones
Management Of Persistent Aki
Persistent AKI occurs in a subset of patients with AKI given the poor outcomes associated with persistent AKI, the ADQI workgroup recommends the presence of persistent AKI as a wake-up call to initiate further assessment and evaluation of treatment options. When a diagnosis of persistent AKI is made, the clinician should reassess the patient carefully and reconsider treatment options. First, the aetiology of the AKI should be considered. In most cases this aetiology is multifactorial, and it will occur secondary to another disease and notably can occur in early, middle, or late phases of the patient’s hospital stay,. A diagnosis of persistent AKI should prompt re-evaluation of the possible causes of AKI, and correction of the underlying cause when possible. Identification of potential causes of AKI might require additional tests such as evaluation of urine sediment, proteinuria, biomarker assessment and/or imaging. In select circumstances, consultation of other specialties might be needed to help diagnose rare causes of AKI .
Prevention Of Acute Kidney Failure
Preventing and treating illnesses that can become the risk factor for AKD is the best way to curb out kidney failure. Upon learning that your kidney function is low, make sure to change a few of your lifestyle habits and do regular physical exercise . Talk to your doctor and take the help of a dietician who can suggest a decent diet to avert kidney failure. A diet is a healthy component of acute kidney disease treatment in Ayurveda!
Get your kidney function tests now!
Kidney Diseases
Read Also: Seltzer Water Kidney Stones
How Can I Prevent Acute Kidney Injury
Because AKI happens suddenly, it can be hard to predict or prevent it. But taking good care of your kidneys can help prevent AKI, chronic kidney disease and kidney failure/ESRD. Follow these general rules to keep your kidneys as healthy as possible:
- Work with your doctor to manage diabetes and high blood pressure.
- Live healthy! Eat a diet low in salt and fat, exercise for 30 minutes at least five days per week, limit alcohol and take all prescription medicines as your doctor tells you to.
- If you take over-the-counter pain medicines, such as aspirin or ibuprofen, do not take more than is recommended on the package. Taking too much of these medicines can hurt your kidneys and can cause AKI.
Preventing Acute Kidney Injury
Those at risk of AKI should be monitored with regular blood tests if they become unwell or start new medication.
It’s also useful to check how much urine you’re passing.
Any warning signs of AKI, such as vomiting or producing little urine, require immediate investigation for AKI and treatment.
People who are dehydrated or at risk of dehydration may need to be given fluids through a drip.
Any medicine that seems to be making the problem worse or directly damaging the kidneys needs to be stopped, at least temporarily.
The National Institute for Health and Care Excellence has produced detailed guidelines on preventing, detecting and managing AKI.
Don’t Miss: Is Wine Bad For Kidney Stones
How Do You Detox Your Kidneys
In the last few decades, kidney detoxing and kidney cleansing programs have gained a lot of popularity. However, so far, there isnt any convincing scientific evidence that cleansing programs do anything.
If there where toxins that are accumulating in your kidneys, that would mean you have uremia, and the only effective detox therapy, in that case, is dialysis.
Just remember drinking water every day and having a healthy diet. That is all the help your kidneys require from you.
What Tests To Perform
Serum creatinine concentration is the main test used to diagnose AKI. In non-steady state conditions such as AKI, the SCr concentration may not provide an accurate estimate of glomerular filtration rate because changes in SCr may lag by many hours. In the setting of AKI, daily measurements of SCr should be performed. More frequent measurements may be indicated in critically ill individuals.
The pattern of rise in SCr may be helpful diagnostically. Pre-renal azotemia usually leads to modest rises in SCr that return to baseline with treatment of the underlying condition. Contrast nephropathy typically leads to a rise in SCr within 24 to 48 hours, a peak within 3 to 5 days, and subsequent resolution within 5 to 7 days. Atheroembolic disease usually shows more subacute rises in SCr, though rapid increases may be observed in severe cases. Increases in SCr of 0.5 mg/dL or greater within 24 hours may reflect substantially reduced kidney function, and such patients should be monitored carefully.
Blood urea nitrogen increases in AKI but can also increase due to hypercatabolic states, upper gastrointestinal bleeding, hyperalimentation, and corticosteroid therapy. A disproportionate rise in BUN compared to SCr, in the absence of other causes of BUN elevation, may be observed in pre-renal azotemia.
Dont Miss: Does Red Wine Cause Kidney Stones
Recommended Reading: Watermelon And Ckd
Management Across The Trajectory Of Aki
In most patients with AKI who receive medical attention and in whom the injury is either self-limited or the underlying cause has been corrected , kidney function begins to improve within 2448hours. However, in 2535% of patients, AKI persists for 72hours. These patients have considerably worse outcomes. Thus, persistent AKI should prompt clinicians to revisit their working diagnosis as to the cause of AKI and re-evaluate the general management principles. For example, a patient who develops AKI following cardiac surgery should have volume status, haemodynamics, and medication list carefully reviewed, and any problems corrected. For most of these patients, this approach will be effective. However, if AKI persists, the clinician should check these points again to ensure that nothing was missed. For clinicians who have little experience in the care of patients with AKI, this might also involve consultation with a nephrologist.
What Is Unique About The Way Yale Medicine Treats Aki
Yale Medicine is at the forefront of detecting acute kidney injury before it happens. Our researchers are looking for reliable biomarkers for the condition and testing real-time electronic alerts for kidney damage. The goal is to determine whos at risk beforehand and prevent it from becoming a problem. Were taking an active role in acute kidney injury, Dr. Wilson says. We believe that by intervening early right when the kidney function starts to decrease that we can mitigate the injury, which could improve outcomes in the long run for patients.
Read Also: Can Kidney Stones Cause Constipation Or Diarrhea
A Framework To Classify Akd And Recovery
Table 1 Recommendations for AKD staging
Finally, in keeping with the original conceptual framework for AKD as proposed by KDIGO, we recognize that AKI might not have always been diagnosed in a patient who appears to have an acute deterioration in renal function. In other words, the diagnosis of AKD may require inference of the existence of an episode of AKI. For example, consider a patient who is seen for an annual internist visit. The patient’s serum creatinine is found to be twice the level observed the year before and they describe a severe ‘flu-like’ illness 2 months prior that lasted a week but eventually resolved without medical attention. We would suggest that treating this situation as a likely case of AKD for example, by requesting that the patient avoids unnecessary nephrotoxins, requesting follow-up serum creatinine measurements, and screening for CKD risk factors would be reasonable.
Who Gets Acute Kidney Injury
Anyone can get AKI. Most of the time, AKI happens in people who are already sick and in the hospital. People who are in the intensive care unit are even more likely than people who are in other units of the hospital to have AKI. This is because people who need to be in the ICU are already very sick. Other things that can increase your risk of having AKI include:
- Being age 65 or above
- Having a kidney disease or kidney problem
- Having high blood pressure
- Having a chronic disease, such as heart disease, liver disease or diabetes
- Having peripheral artery disease
Don’t Miss: Acv And Kidneys
Kidney Damage Treatment Options
There are two levels of healthcare to treat kidney damage, depending on the severity of the kidney damage. In cases where damage is acute, or minimal, its possible to treat the complications of the disease with medication until lifestyle changes can be made.
However, in the case of severe or end-stage kidney damage, the only treatment options are dialysis and kidney transplant.
Before any treatment for kidney damage, we highly recommend talking to your trusted healthcare professional, as they can determine exactly the stage of your kidney damage and the best solution.
Complications Of Acute Kidney Injury
The most serious complications of acute kidney injury are:
- high levels of potassium in the blood in severe cases, this can lead to muscle weakness, paralysis and heart rhythm problems
- fluid in the lungs
- acidic blood which can cause nausea, vomiting, drowsiness and breathlessness
Page last reviewed: 25 February 2019 Next review due: 25 February 2022
Also Check: Constipation And Kidney Stones
Direct Kidney Damage Or Kidney Trauma
Some types of injury, diseases, or conditions can damage your kidneys and lead to AKI, including:
- Physical injury
- Vasculitisa rare blood vessel condition
- Allergic reactions to certain drugs
- Illegal drugs or some prescription medications
- Diseases of connective tissue called scleroderma
- Inflammation or damage to blood vessels in the kidneys
Box 1 Selected Causes Of Aki
Pre-renal causes, impaired renal perfusion
Cardiorenal syndrome, including heart failure with reduced ejection fraction, right-sided heart failure and venous congestion
Shock, including haemorrhagic shock, hypovolaemic shock and septic shock
Abdominal compartment syndrome
Kidney transplant, including delayed graft function
Medication, including angiotensin-converting enzyme inhibitors and angiotensin receptor blockers
Intra-renal causes
Thrombotic microangiopathies, cholesterol embolism, anti-glomerular basement membrane disease and immune complexes and anti-neutrophilic cytoplasmic autoantibody vasculitis
Sickle cell anaemia and sepsis
Systemic infections and sepsis, pyelonephritis, drug-related or heavy metal-related tubule necrosis, crystal-induced nephropathy , myoglobin , contrast media, light chains and metabolites
Acute cellular rejection, acute interstitial nephritis, immune checkpoint inhibitor-related and cytokine release syndrome upon chimeric antigen receptor T cell therapy
Post-renal causes, urinary tract obstruction
Bilateral ureteral obstruction, bladder dysfunction and urethral obstruction
AKI, acute kidney injury.
Recommended Reading: Aleve Effect On Kidneys
Kidney Injury And Recovery
Fig. 4: Main principles of the pathophysiology of AKI.
Many other triggers can cause ATN , but combinations of triggers are common, especially in ICU settings. Human data are scarce but animal models suggest that ATN is not a passive process but instead involves different forms of regulated necrosis, such as necroptosis and ferroptosis, that can synchronize tubular cell death along entire tubule segments and spares glomeruli,. The necrotic tubular cells can form casts and obstruct the lumen of tubules. Tubule necrosis involves the release of danger signals that activate Toll-like and other pattern recognition receptors on resident immune cells in the kidney interstitium, namely MHCII+F4/80Hi conventional dendritic cells in mice however, little is known about the immune cell dynamics in human AKI. Activation of these cells triggers the influx of neutrophils in the early injury phase and M1 macrophages and other myeloid cells in the late injury phase, which all contribute to a local inflammatory response that accelerates tubule necrosis, an auto-amplification loop referred to as necroinflammation,. Unless the nephrotoxic trigger persists, as in persistent ischaemia, toxin exposure or alloimmunity, numerous counter-regulators support a resolution of necroinflammation, which is a requirement to launch healing responses.
Original Articlemild Elevation Of Urinary Biomarkers In Prerenal Acute Kidney Injury
Prerenal acute kidney injury is thought to be a reversible loss of renal function without structural damage. Although prerenal and intrinsic AKI frequently coexist in clinical situations, serum creatinine and urine output provide no information to support their differentiation. Recently developed biomarkers reflect tubular epithelial injury therefore, we evaluated urinary biomarker levels in an adult mixed intensive care unit cohort of patients who had been clinically evaluated as having prerenal AKI. Urinary L-type fatty acidbinding protein , neutrophil gelatinaseassociated lipocalin , interleukin-18 , N-acetylD-glucosaminidase , and albumin in patients with prerenal AKI showed modest but significantly higher concentrations than in patients with non-AKI. We also conducted a proof-of-concept experiment to measure urinary biomarker excretion in prerenal AKI caused by volume depletion. Compared with cisplatinum and ischemiareperfusion models in mice, volume depletion in mice caused a modest secretion of L-FABP and NGAL into urine with more sensitive response of L-FABP than that of NGAL. Although no histological evidence of structural damage was identified by light microscopy, partial kidney hypoxia was found by pimonidazole incorporation in the volume depletion model. Thus, our study suggests that new AKI biomarkers can detect mild renal tubular damage in prerenal acute kidney injury.
- Previous article in issue
Also Check: Can You Have 4 Kidneys
Also Check: Is Almond Milk Bad For Kidney Stones