Vitamin D In The Treatment Of Aki
Many studies have been performed mainly with rats to define the potential use of VitD as treatment for AKI .
A dominant cause of AKI is IRI, induced by the actuation of inflammation and the increased expression of matrix metalloproteinases . Ersan et al. studied the effect of paricalcitol on MMPs expression and, subsequently, on IRI progress. Pre-treatment with paricalcitol resulted in amelioration of IRI-AKI via an MMP-dependent inflammatory mechanism .
Hamzawy et al. studied the effect of pre-treatment with 22-oxacalcitriol on IRI-AKI and found that it can ameliorate AKI through: an anti-inflammatory mechanism via inhibition of Toll-like receptor-4 and interferon- , a reduction of Na+/H+ exchanger-1 , a pro-autophagic action via elevating Beclin-1 expression and LC3II/LC3I ratio, an anti-apoptotic action via elevating Bax/Bcl-2, cytochrome c and caspase-3 expression, and an inhibitory action on G1 cell cycle arrest via reducing insulin-like growth factor-binding protein-7 and tissue inhibitor of matrix metalloproteinases-2 expression .
In another study, Kapil et al. also investigated the protective role of VitD pre-treatment in IRI-AKI and showed a renoprotective effect in IRI against oxidation and lipid peroxidation mediated by peroxisome proliferatoractivated receptor- – .
Yes You Can Take Too Many Vitamins: Man Damages Kidneys With Too Much Vitamin D
- Copy article linkCopy link
A lot of Canadians take vitamin D, particularly during the dark winter months. But you can get too much of a good thing one man developed permanent kidney damage after taking high doses of the sunshine vitamin, according to a recent case study.
The case report, published Monday in the Canadian Medical Association Journal, highlights the risks of too much vitamin D.
According to the report, a 54-year-old man had his kidneys examined after a routine blood test found he had very high levels of creatinine a waste product produced during normal muscle function. High levels of creatinine in the blood can indicate kidney trouble, since the product is normally filtered out by the kidneys.
READ MORE: Vitamins wont prevent a heart attack or make you live longer, study finds
Doctors were baffled at first, as the mans kidney function was at less than 15 per cent for no apparent reason, according to Dr. Bourne Auguste, a clinical fellow in nephrology at Toronto General Hospital and a co-author of the report.
WATCH: The role of vitamin D for people living with MS
Healthy adults under age 50 should have only 400-1,000 IU daily, according to Osteoporosis Canada. A dose of 800-2000 IU is recommended for people at high risk of bone fractures and osteoporosis. This patient was not a high-risk individual.
READ MORE: Vitamin D supplements arent helping your bones, study finds
No one would ever be on these doses for years at a time, he said.
How Do You Know If Youve Got Low Vitamin D Levels
Great question! Depending on how low your levels are, you might notice any of the following signs: frequent infections, fatigue, bone and back pain, low mood, impaired wound healing, hair loss and muscle pain.
The thing is, many of these signs could be related to other conditions so the best way to figure out if you are deficient in vitamin D is to have a blood test checking your vitamin D levels.
Read Also: What Is The Va Disability Rating For Kidney Disease
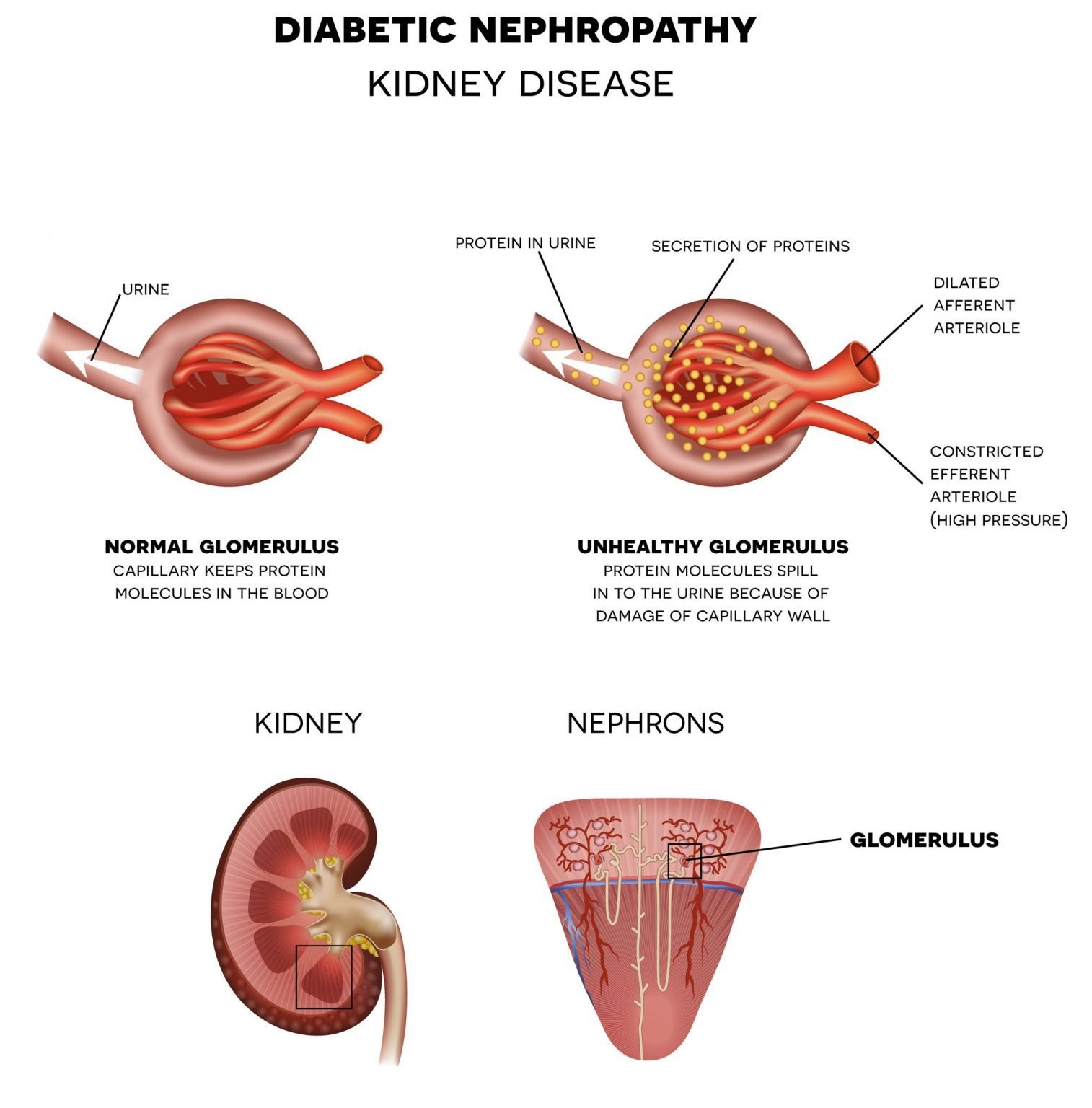
D Levels And Renal Hyperfiltration In Korean Adults: Jhee Et Al
Jhee et al. investigated the association between renal hyperfiltration and vitamin D status in a healthy Korean population. The authors used the 4th, 5th, and 6th editions of the Korean NHANES , a nationwide population-based cross-sectional study from 2008 to 2015. After applying their exclusion criteria, they ended up studying 33,210 subjects with estimated glomerular filtration > 60 mL/min1/1.73 m2. They defined vitamin D deficiency as a serum 25D concentration < 20 ng/mL and severe vitamin D deficiency as < 10 ng/mL . Serum 25D concentrations between 20 and 29.9 ng/mL were defined as vitamin D insufficient , whereas concentrations 30 ng/mL were defined as sufficient . Earlier studies showed that South Korean post-menopausal women have relatively lower 25D levels compared to women from other countries, so this population may be unique in the low prevalence of vitamin D sufficiency .
The mean age of the population was 48.1 years 56.5% were female. The population was relatively healthy with hypertension in only 18%, diabetes mellitus in 6.6% and proteinuria in only 2.5% . In the study, estimated GFR was calculated using the Korean version of the CKD-Epi equation. A logarithm transformed eGFR in the 95th percentile or greater, after adjustment for age, sex, height, weight, and history of hypertension or diabetes was considered to be renal hyperfiltration.
Vitamin D Deficiency In Ckd
Recent observations have demonstrated that kidney disease seems to be associated with a high incidence of vitamin D insufficiency or deficiency . Studies by Gonzalez et al. demonstrated that 25-hydroxyvitamin D values are < 30 ng/ml, believed be the lower limit of normal, in the majority of patients with CKD. Patients who are severely proteinuric have the lowest values. These investigators have shown that virtually all of the secondary hyperparathyroidism that occurs in the course of CKD is associated with 25-hydroxyvitamin D values that are < 30 ng/ml. It is interesting to note that in this patient group, there is a positive relationship between 25-hydroxyvitamin D levels and 1, 25-dihydroxyvitamin D levels, in contrast to what is seen in normal individuals. Thus, when 25-hydroxyvitamin D levels are increased by therapy, one would anticipate an increase in the levels in the 1,25-dihydroxyvitamin D. It is not clear whether this is a contribution of renal 1–hydroxylase or the 1–hydroxylase at extrarenal sites however, because of the association of low levels of 25-hydroxyvitamin D with hyperparathyroidism in the course of CKD, it is recommended that in patients with CKD, if hyperparathyroidism is detected, then 25-hydroxyvitamin D should be measured, and if found to be < 30 ng/ml, then the initial step in the therapy should be to try to correct this abnormality, as the first step in the control of hyperparathyroidism.
Don’t Miss: How To Flush Kidneys And Bladder
Definition: Vitamin D Deficiency Vitamin D Sufficiency Chronic Kidney Disease
VD status is being evaluated via the serum level of 25-hydroxyvitamin D the metabolite formed in the first hydroxylation in the liver, due to its longer half-life , compared to the active metabolite 1,25-dihydroxyvitamin D . The best options for 25VD serum level evaluation methods are high performance liquid chromatography and liquid chromatography-tandem mass spectrometry . There are reports, discussing the use of free 25VD as indicator of VD status. However, in renal disease, the ratio between free and total 25VD remained unchained therefore, total 25VD is the indicator of VD status in CKD .
Generally, 25VD level has reverse association with parathyroid hormone levels. In addition, higher 25VD is associated with higher calcium intestinal reabsorption. However, at 25VD 75 nmol/l, no reduction in PTH levels and no increase in calcium intestinal reabsorption occurs . Therefore, 25VD 75 nmol/l is regarded as a cut-off value for vitamin D sufficiency.
No generally accepted definition for VD deficiency exists, as authors choose cut-off value either serum 25VD of 25 nmol/L or serum 25VD of 50 nmol/L . However, target levels of 75 nmol/L are recommended, taking into consideration the clinical importance of mild VD insufficiency .
Chronic kidney disease is defined as abnormalities of kidney structure or function, present for more than 3 months, with implications for health . CKD patients are at increased risk for VD deficiency therefore, they require VD screening .
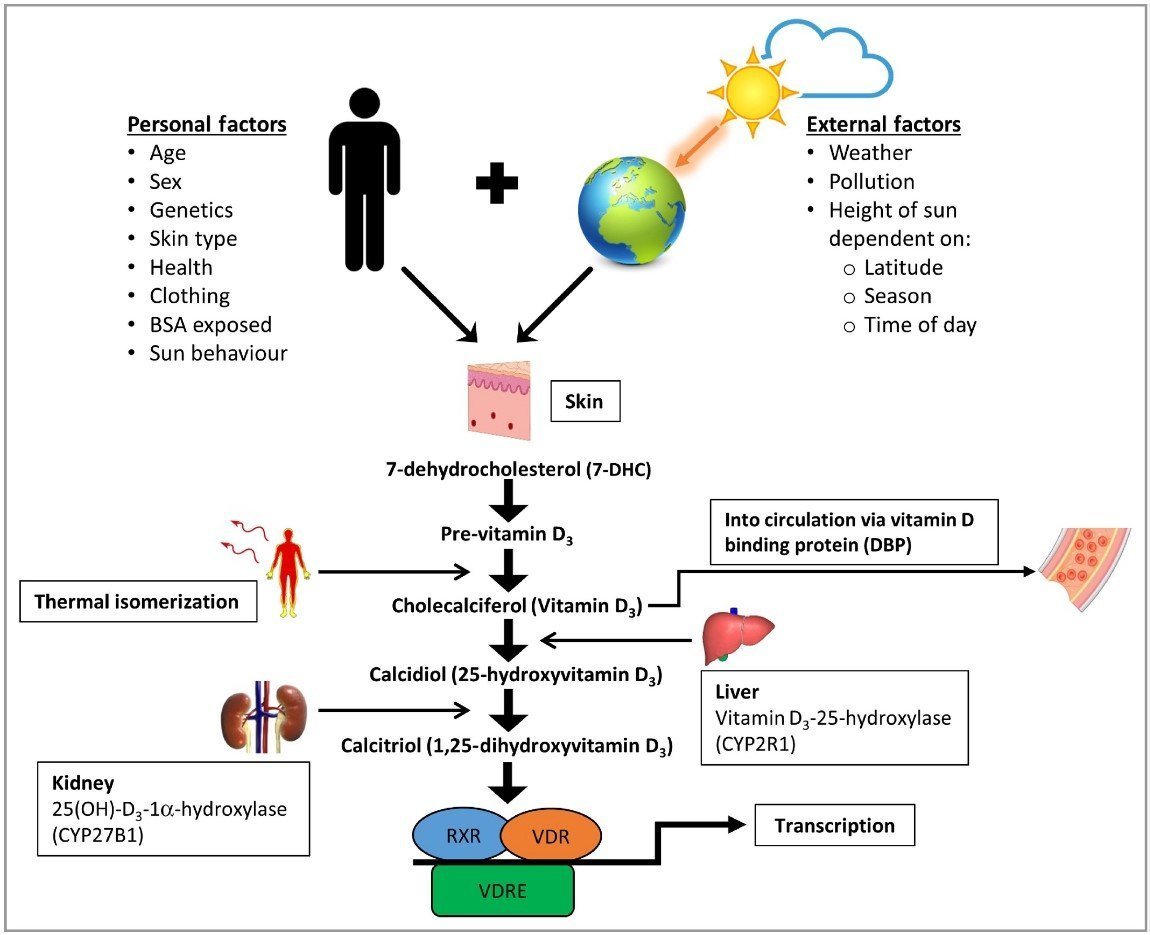
Vd Metabolism In Healthy Subjects
VD is synthesized predominantly endogenously . In the skin, the ultraviolet light transforms 7-dehydroxycholesterol to pre-vitamin D, which under the influence of body temperature spontaneously isomerizes to cholecalciferol . Approximately, 10% of total body VD is taken orally . VD is transported via VD-binding protein to the liver, where it is hydroxylated to 25VD. The next step in VD activation is hydroxylation of 25VD by the enzyme 1-hydroxylase to 1,25VD, which is the active VD metabolite. The process occurs predominantly in the renal tubules. In addition, non-renal CYP27B1 was detected in skin , lymph nodes , colon , pancreas , adrenal medulla, brain , prostate epithelial cells, and placenta , indicating the wider significance of the VD metabolites. Finally, 1,25VD is inactivated by the enzyme 24-hydroxylaze.
The above-mentioned stages of VD metabolism form the so called VD axis.
Recommended Reading: Water In Kidney Symptoms
Rcts With Calcifediol Supplementation
In recent years, preparations of the 25 hydroxylated form of vitamin D, i.e. 25D or calcifediol were developed for oral administration. There are three forms calcifediol and the extended release formula, provided as capsules and the immediate release , provided as a liquid or capsule. The pharmacokinetic profile differs from the parent compound vitamin D. Intestinal absorption of 25D is known to be more efficient and is not dependent on fat absorption, the increase in plasma 25D is more rapid and the doseresponse higher than that of the parent compound. The IR calcifediol formulation was approved in the USA in 1980 for treatment of CKDMBD in dialysis patients . However, it was withdrawn from the market in 2002, since it failed to show meaningful reduction of PTH in patients with CKD G34. IR calcifediol is still available in Europe and licensed for use in various conditions including vitamin D deficiency rickets, renal osteopathy and hypocalcaemia . ER formulations of 25D are only available in the USA at the moment . In 2016 ER calcifediol was approved in the USA to treat SHPT in adult CKD patients G34 and vitamin D insufficiency . Studies in CKD patients showed that ER calcifediol results in a slower increase of 25D levels, more significant suppression of iPTH and less of an increase of 24,25D compared to IR-calcifediol .
What Happens To Pth In Kidney Disease
People with more advanced kidney disease may have elevated PTH. This excess of PTH tells the body to pull calcium out of the bones and put it in the bloodstream which can result in bone pain and weak bones that fracture easily as well as calcium build up in tissues and organs such as the heart and blood vessels.
Vitamin D deficiency is one of the causes of secondary hyperparathyroidism.
If I havent already impressed on you the importance of maintaining optimal vitamin D levels here are a few more of the reported benefits of vitamin D supplementation for people with kidney disease:
- Serum parathyroid hormone levels decrease
- Reduced proteinuria
- Increased red blood cell production and iron levels
- Slower progression of kidney disease and improved survival
You May Like: Cranberry Good For Liver
Is It Better To Take Vitamin D Every Day Or Once A Week
Current guidelines say adults shouldnt take more than the equivalent of 100 micrograms a day. But vitamin D is a fat-soluble vitamin, so your body can store it for months and you dont need it every day. That means you could equally safely take a supplement of 20 micrograms a day or 500 micrograms once a month.
Is Sweet Potatoes Bad For Kidney Disease
Sweet potatoes also contain vitamins and minerals, such as potassium, that may help balance the levels of sodium in the body and reduce its effect on the kidneys. However, as sweet potato is a high-potassium food, anyone who has CKD or is on dialysis may wish to limit their intake of this vegetable.
Also Check: What Laxative Is Safe For Kidneys
Vitamin Cocktails May Injure Kidneys
Athletes seeking a competitive edge may turn to performance-enhancing substances, but people using these chemicals often experience tragic results.
A January 2017 review in Nefrologia described 16 cases of vitamin cocktail abuse by body sculptors.
These people injected a veterinary product with a mix of vitamins A, D and E, and all ended up in the hospital with acute kidney injury. Doctors restored kidney function in some, but not all, cases.
Vitamin cocktails can also increase the risk of vitamin-drug interactions. For example, a December 2014 report in Nutrition Research Reviews describes how vitamin E alters the effects of common medicines like cyclosporine A, warfarin and aspirin.
People with diabetes who have kidney damage may seek to restore their health by taking vitamin D, and researchers have shown that vitamin D may help hide diabetic symptoms. An August 2017 paper published in Drug Development Research showed that this nutrient increased insulin sensitivity in an animal model of diabetes, but unfortunately, the vitamin D administered also caused kidney damage.
Such a result is not surprising. Scientists classify vitamin D as a fat-soluble vitamin. It can, therefore, accumulate in the body and cause hypervitaminosis.
Read More: How Does Diabetes Occur?
The Role Of Vitamin D In Kidney Disease
Duncan Capicchiano
Vitamin D deficiency is the most common nutrient deficiency in the world and is particularly common in people with kidney disease. Add to that the fact that vitamin D deficiency is linked to progression of kidney disease and increased risk of mortality and I think we have a few pretty good reasons to explore the role vitamin D and the importance of maintaining optimal vitamin D levels.
Interestingly enough, vitamin D is completely different than any other vitamins. In fact, its not really a vitamin at all! Vitamin D is actually a prohormone- a nutrient that converts into a hormone within the body.
Being a fat-soluble vitamin, vitamin D is stored in the body in fat cells which can be accessed as needed.
Read Also: What Laxative Is Safe For Kidneys
Where Do You Get Vitamin D From
The short answer is from food, the sun, or supplements.
Few foods contain sufficient vitamin D so most of it is made in our body after exposure to sunlight.
When our skin is exposed to sunlight, or rather, the ultraviolet B radiation that the sun emits, it makes vitamin D from cholesterol. The amount of vitamin D your skin makes depends on the season, the time of day, where you live, your age and the melanin content of your skin- the darker your skin the more sun exposure you need to make sufficient vitamin D.
Like all other vitamins we do get some vitamin D from food, but they dont contain large enough amounts to be our primary source.
There are two main dietary forms of vitamin D:
- Vitamin D3 – found in some animal foods, like fatty fish and egg yolks.
- Vitamin D2 – found in some plants, mushrooms and yeasts.
Mechanisms Of Altered Vitamin D Metabolism In Kidney Disease
There seem to be several mechanisms involved in the decreased levels of 1,25-dihydroxyvitamin D that occur in the course of kidney disease . Thus, a decrease in renal mass will obviously limit the quantities of 1–hydroxylase that are available for production of the active vitamin D metabolite. A reduction in GFR may limit delivery of substrate to the 1–hydroxylase, which may also limit the ability of the kidney to produce 1,25-dihydroxyvitamin D. The importance of a declining GFR in limiting the ability of the kidney to produce 1 to 25-dihydroxyvitamin D was illustrated by the work of Nykjaer et al. , who demonstrated that glomerular filtration of 25-hydroxyvitamin D, bound to vitamin Dbinding protein, undergoes glomerular filtration and uptake into the proximal tubule cell by the receptor megalin and was the rate-limiting step in the delivery of 25-hydroxyvitamin D to the 1–hydroxylase enzyme. Accordingly, as GFR declines, there is a limitation of substrate delivery that can compromise the ability of the failing kidney to produce 1,25-dihydroxyvitamin D . This may be compounded by the decreased levels of 25-hydroxyvitamin D that seem to be common in patients with kidney disease .
Figure 1.
Diagram of the mechanisms involved in limiting the ability of the kidney to maintain the levels of 1,25-dihydroxyvitamin D in chronic kidney disease . C-PTH, C-terminal parathyroid hormone FGF-23, fibroblast growth factor-23 Pi, phosphate.
Also Check: Can You Have 4 Kidneys
Vd Pleiotropy After Kidney Transplantation
The graft survival at the tenth year after KT is significantly lower than the survival during the first 12 months. The explanation for these unsatisfactory results is poorer patient survival due to neoplasia, CVD, NODAT, calcineurin toxicity. It could be hypothesized that VD can improve graft and patient survival due to its pleiotropy. However, the trials in KTRs are small in number and in size, thus further research in this sphere is warranted.
5.2.1 VD pleiotropy after KT: proteinuria and renal protection
Observational studies linked poor VD status to poorer graft outcomes . Our results also demonstrated that higher VD is associated with lower post-transplant proteinuria . However, interventional studies did not fully support the VDgraft function association. Cholecalciferol supplementation failed to demonstrate renoprotection in prospective study . However, in a recent prospective placebo-controlled study, paricalcitol ameliorated proteinuria in KTRs .
5.2.2 VD pleiotropy after KT: rejection
Observational studies demonstrated higher rates of acute rejection in VD deficient KTRs . Unfortunately, interventional studies did not find protective role of cholecalciferol supplementation on rejection prevalence . Therefore, the role of VD in rejection prevention after KT is not fully understood and is under debate.
5.2.3 VD pleiotropy after KT: infection
5.2.4 VD pleiotropy after KT: malignancies
5.2.5 VD pleiotropy after KT: NODAT
What Makes Creatinine High
Generally speaking, high levels of creatinine can indicate that your kidneys arent working well. There are many possible causes of high creatinine, some of which may be a one-time occurrence. Examples can include things such as dehydration or intake of large amounts of protein or the supplement creatine.
Don’t Miss: Pomegranate Juice For Kidney Stones
Rcts With Vitamin D Supplementation
Vitamin D is the inactive precursor of 1,252D and exists in two forms, vitamin D3 and D2 . Vitamin D is the most commonly used form for the prevention and treatment of deficiency in both the general population and patient groups. Vitamin D3 supplementation leads to a somewhat longer sustained increase of 25D, but otherwise the metabolism of D3 and D2 is identical.
Nine of the RCTs included in this systematic review used vitamin D3 or D2 supplementation . All studies has a small sample size . In some of these studies the group that received Vitamin D served as the reference group. They were all conducted with CKD patients stages 34. The doses varied from 2000 to 4000 IU daily or 40,00050,000 IU weekly and the duration was between 1 and 12 months. All nine studies found a significant increase in plasma 25D concentrations. Four of these studies observed a significant reduction of PTH, whilst in the remaining five, no significant change of PTH in response to the vitamin D supplementation was found . The small sample sizes, differences in dosages and duration of supplementation may explain these inconsistent results higher doses show to be more effective in suppressing PTH. Only five of these studies provided sufficient detail for inclusion in meta-analysis, which showed a non-statistically significant decrease in PTH of 18 pg/mL . When also two studies with calcifediol were considered, the effect on PTH was highly significant , but heterogeneity was substantial .