Assessing The Predictive Value Of Icd
In both health boards over the whole period studied, sensitivity of ICD-10 coding compared with gold standard biochemically defined AKI was poor for all stages of AKI and for Stages 2 and 3 AKI . Positive predictive values were moderate or poor for all AKI and for Stage 2 and 3 AKI . Specificity and negative predictive value over the whole period studied were both consistently high .
In Tayside, there was an increased proportion of coded AKI consisting of AKI Stage 1 following the introduction of the AKI e-alerts but a non-significant reduction in those with biochemically defined AKI . In NHS Fife, where e-alerts were not introduced, there was a similar increase in the proportion of coded AKI consisting of AKI Stage 1 for the same time frame , though there was a small increase in those with biochemically defined AKI .
In Tayside, with N17-coded AKI, sensitivity was 23.7% before the introduction of the alerts and 27.9% after the introduction of the alerts. For more severe AKI, pre-intervention sensitivity was 42.6% and post-intervention was 45.2% . In NHS Fife, sensitivity of N17 was 33.2% before the introduction of the alerts in Tayside and 39.1% after the introduction of the alerts. For more severe AKI stages, pre-intervention sensitivity was 51.4% and post-intervention sensitivity was 57.1% .
Sensitivity before and after Tayside e-alert introduction of ICD-10 code N17 for biochemically defined AKI
| Health board . |
|---|
Interrupted Time Series And Segmented Regression Analysis Of Change In Icd
The pre- and post-intervention rates were plotted over time, as shown in . Over the course of the study, 31/1000 of NHS Tayside inpatients were coded with ICD-10 code N17 compared with 35/1000 in NHS Fife. Results of segmented regression analysis for NHS Tayside showed that there was no significant change in level at the time of the introduction of the e-alerts and the change in trend indicated that coded AKI rates had in fact fallen since the introduction of the alerts compared with prior trends . The absolute change at 24-months post-intervention was 9.5 and the relative change was 27.0% , with the overall effect being a flattening of the previous rising trend. Results for NHS Fife demonstrated that there was no change in either level or trend over the course of the study .
Effect Of Baseline Proteinuria On The Association Between Aki And Subsequent Ckd Progression
A key parameter that characterizes the severity of chronic kidney disease in addition to estimated GFR is the level of proteinuria. James et al. utilized a provincial sample of nearly one million adults in Alberta, Canada to study the associations among baseline renal function, proteinuria, and AKI.20 While they found that lower baseline estimated GFR and higher levels of proteinuria were associated with a greater risk of AKI, they also observed that higher levels of proteinuria predicted the long-term renal composite outcome of ESRD or doubling of serum creatinine, following an episode of AKI . This study has provided important evidence that proteinuria worsens, in an additive and graded manner, the impact of AKI on long-term renal function decline across all levels of baseline estimated GFR.20
Rate ratios of the composite outcome of end-stage renal disease or doubling of serum creatinine after acute kidney injury by baseline kidney function and proteinuria, reproduced with permission by James, et al.20
Blue squares and horizontal bars represent point estimates and 95% CIs respectively for rate ratios of participants who had AKI for various values of eGFR and proteinuria. Red squares and horizontal bars similarly represent the point estimates and 95% CIs for participants who did not have AKI. The referent group for all rate ratios are participants who did not have AKI, and had normal proteinuria and eGFR 60 ml/min/1.73m2.
Recommended Reading: Pomegranate Juice Good For Kidney Stones
Who Is It Intended For
The Kidney disease solution program can be beneficial for people with kidney issues with limited options for dealing with their kidney problems. If you suffer from kidney issues, you may consider trying the program and see the positive impact it has for your overall health. For those who are in the late stages of kidney disease it could even reverse your condition.
If you dont suffer from kidney disease, you may still want to try the program since everyone can benefit from the suggestions as well as recipes and workouts that are included in the program. Its not just about improving kidney function but also improving lifestyle and diet for greater overall health. After all prevention is always more effective than treatment.
However, those with medical conditions should consult first with their physician prior to taking the program. This program is not suitable for pregnant women nursing mothers, or anyone under the age of 18 years old.
Diagnosis For Renal Failure
For a complete diagnosis of renal failure, a complete medical history is taken followed by a physical examination. The following tests are done to determine renal failure:
- Blood tests: This is necessary to determine electrolyte levels, blood cell count and the kidney functioning
- Urine test: This will also help in determining the functioning of the kidneys
- Ultrasound or sonography: In sonography, sound waves are passed over the abdomen in the area of kidney. These sound waves form an image on the screen, which help in determining the size, shape and any anomalies in the kidney. Any mass, stone, cyst or obstruction can be detected by this method.
- Biopsy: A small tissue sample of the kidney is taken by means of a needle or during surgery. This tissue sample is then checked under microscope for any abnormalities, especially cancerous growth or presence of abnormal cells.
- CT scan: Computed tomography is done using X-rays and computers to generate images in the form of thin slices of the body. It helps in showing detailed images of the body parts and can be used on all body parts like bones, fats, muscles, etc. They are much more detailed than normal X-Rays.
Recommended Reading: Is Ibuprofen Metabolized In The Kidneys Or Liver
Poa For Chronic Kidney Disease Stage 3 Progressing To End Stage Renal Disease
The patient was admitted with acute respiratory failure, acute kidney injury due to acute tubular necrosis and chronic kidney disease, stage 3. The patient had a prolonged hospitalization and during the hospital course, he advanced to end stage renal disease and was started on hemodialysis. The provider stated, Concerning possible renal recovery, it appears unlikely he will ever be dialysis independent given his history of CKD prior to his acute on chronic kidney injury and also because he is almost three months from his initial renal insult with no signs of renal recovery. Since the chronic kidney disease, stage 3 had progressed to ESRD, requiring dialysis, what is the appropriate present on admission indicator for the ESRD?…
To read the full article, sign in and subscribe to AHA Coding Clinic® for ICD-10-CM and ICD-10-PCS .
Access to this feature is available in the following products:
|
Acute Kidney Failure Unspecified
- 2016201720182019202020212022Billable/Specific Code
- N17.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM N17.9 became effective on October 1, 2021.
- This is the American ICD-10-CM version of N17.9 – other international versions of ICD-10 N17.9 may differ.
type 2 excludes
- traumatic kidney injury (
- 2016201720182019202020212022Non-Billable/Non-Specific Code
Type 2 Excludes
- Applicable To annotations, or
Recommended Reading: Is Apple Cider Vinegar Good For The Kidneys
Conflict Of Interest Statement
None declared. All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf. R.L., P.D., N.D.S., B.G., D.B. and S.B. declared that no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Nursing Diagnosis For Chronic Renal Failure
Chronic renal failure happens when there is progressive and gradual loss of kidney functioning. The progress is usually so slow that the symptoms are not visible till the kidneys almost stop working.
1. Risk for Decreased Cardiac Output
This can be a result of reduced circulating volume, systemic vascular resistance and myocardial workload.
Interventions
- Check for lung and heart sounds, presence of edema, dyspnea and congestion.
- Check for signs of hypertension, postural changes in blood pressure.
- Check for chest pain, activity level assessment and response to activity.
- Chest X-rays can be taken, monitoring of blood parameters should be done.
2. Risk for Ineffective Protection
An abnormal blood profile which includes decreased RBC, changes in clotting factor, and increased capillary fragility can put a person at risk of ineffective protection.
Interventions
- Check level of consciousness, changes in behavior, ability to perform given tasks, any reports of weakness or fatigue.
- Provide assistance when required, check venipuncture sites for swelling, bleeding.
- Monitor lab reports, check stool test report, give fresh blood as required.
3. Disturbed Thought Process
Accumulation of toxins like urea in the blood can cause electrolyte imbalance, metabolic acidosis and calcifications in the brain. Symptoms may include disorientation as to time, place and person, reduced attention span, memory loss, inability to make decisions, changes in behavior, and coma.
Interventions
Interventions
You May Like: Can Carbonated Water Cause Kidney Stones
Q& a: Reporting Acute Renal Insufficiency Due To Dehydration In Icd
Q: Our team is having trouble deciding how to report a recent case. We have a patient who presented with a two-day history of nausea, vomiting, and diarrhea. The patient is showing symptoms of fatigue and dehydration. Lab values show hyperkalemia, acidosis, and elevated serum creatinine and blood urea nitrogen levels. The patient is diagnosed as having acute renal insufficiency due to dehydration with decreased urinary output and was admitted for IV hydration. What diagnosis codes should we assign?
A: The ICD-10-CM codes that would be most appropriate for this case are:
- N28.9, disorder of kidney and ureter, unspecified
- E86.0, dehydration
ICD-10-CM code N28.9 is reported to capture the acute renal insufficiency. Based on your documentation, acute kidney injury/failure cannot be assigned. However, based on the clinical indicators documented, a query should be submitted to the provider to specify if the type of acute renal insufficiency is acute kidney injury/acute renal failure.
Editors note: Sarah Humbert, RHIA, AHIMA-certified ICD-10-CM/PCS trainer, coding and compliance manager at KIWI-TEK, LLC, and Temeka Davis, RHIT, coding manager at KIWI-TEK, LLC, answered this question during HCPros webinar Acute Kidney Injury and Acute Renal Failure: 2018 Coding, Criteria, and Classifications.
This answer was provided based on limited information. Be sure to review all documentation specific to your own individual scenario before determining appropriate code assignment.
What Is The Icd 10 Code For Acute On Chronic Kidney Disease
Chronic kidney diseaseICD10code
. Subsequently, one may also ask, how do you code acute on chronic kidney disease?
Code the AKF as primary with ICD-9-CM code 584.9, followed by the stage of CKD prior to the exacerbation. The tip is adapted from Simplify chronic kidney disease outpatient coding in the October Briefings on APCs.
Also Know, what is diagnosis code n179? N179 – Acute kidney failure, unspecified – as a primary diagnosis. N179 – Acute kidney failure, unspecified – as a primary or secondary diagnosis code. Total National Projected Hospitalizations – Annualized 359,000.
Subsequently, question is, what is the ICD 10 code for kidney injury?
S37.0
What does acute kidney failure unspecified mean?
Acute kidney failure occurs when your kidneys suddenly become unable to filter waste products from your blood. When your kidneys lose their filtering ability, dangerous levels of wastes may accumulate, and your blood’s chemical makeup may get out of balance.
Recommended Reading: Is Apple Cider Vinegar Good For Kidneys
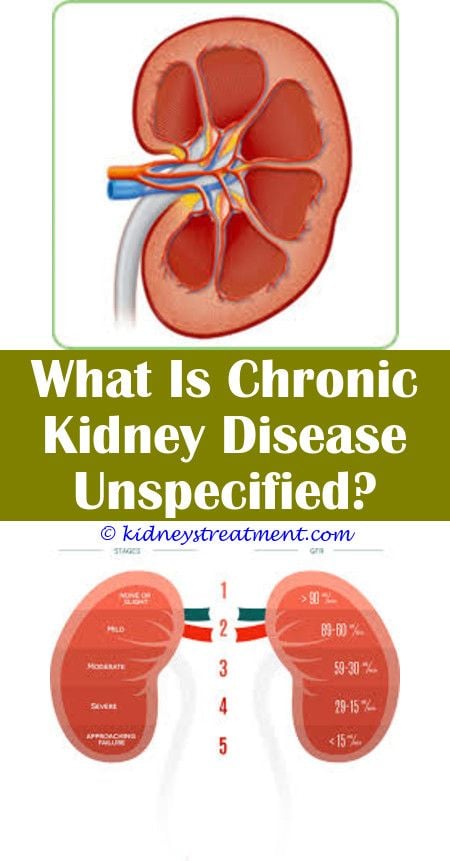
Physiology Is The Key To Better Diagnosis Coding
- Risk, Injury, Failure, Loss of Kidney Function, and End-stage Kidney Disease
- Acute Kidney Injury Network and
- Kidney Disease Improving Global Outcomes .
| Stage | |
| Kidney failure | < 15 |
| Chronic kidney disease is defined as either kidney damage or < 60 mL/min/1.73 m2 for 3 months. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies. |
Source: www2.kidney.org/professionals/KDOQI/guidelines_ckd/p4_class_g1.htmCoding the Stages of CKDThe appropriate code for stages 1-5 is assigned to depict the documented severity of CKD:
- Stage 1 codes to N18.1 Chronic kidney disease, stage 1 .
- Stage 2 codes to N18.2 Chronic kidney disease, stage 2 ).
- Stage 3 codes to N18.3 Chronic kidney disease, stage 3 , ).
- Stage 4 codes to N18.4 Chronic kidney disease, stage 4 , ).
- Stage 5 codes to N18.5 Chronic kidney disease, stage 5, .
Nancy Reading, RN, BS, CPC, CPC-P, CPC-I, has held a Registered Nurse license for 36 years, earned a Bachelor of Science in Biology/Chemistry, and has 26 years of coding experience. She has worked the gamut of the industry, from a large university practice with over 1,000 providers to Medicaid. Reading is a member of the Salt Lake South Valley, Utah, local chapter.
Icd 9 Code For Acute On Chronic Kidney Disease
Many millions of Americans are estimated to have chronic Kidney Disease. In the majority of cases dialysis and kidney transplant are the only choices for patients in advanced stage of the disease.
Enter the Kidney Disease Solution, an all-in-one manual for improving kidney health and functioning. It was created by Duncan Capicchiano and his wife Fiona Chin, the program aims to guide users to stop kidney disease using natural methods.
This thorough review will go over everything you need to learn about the program from how it works to the advantages and costs. If youre wondering whether this program is a good fit for you, then go through the article.
Before you go on, you may want to check out this video by Review Vid on YouTube that gives a quick review. Afterward, you will want to read the rest of our article for a more comprehensive review.
Read Also: Does Chocolate Cause Kidney Stones
The New Codes Are As Follows:
- N18.30 CKD, Stage 3 unspecified
- N18.31 CKD, Stage 3a
- N18.32 CKD, Stage 3b
Kidney disease is often asymptomatic and occurs just before kidney failure. About one-third of the population of older adults have CKD Stage 3. When someone is experiencing Stage 3, it means their kidneys are filtering about half of what they should be, allowing for some fluids, electrolytes, and waste to build up in the body.
CKD often starts to develop without notice. However, symptoms may appear in Stage 3. For those that do experience symptoms, these may include fatigue, swelling around the ankles or eyes, unusually light-colored urine, urinating more frequently, and loss of appetite.
Once an individual has Stage 3 CKD, its generally considered to be irreversible. Fortunately, the majority of Stage 3 patients do not progress to the more severe stages. Still, it is important to work with a doctor to manage the condition and gain a clear picture in regard to the GFR and kidneys. This helps to identify the need for kidney replacement therapy sooner and essentially helps to keep the patient healthier longer.
References:
Effect Modification By Baseline Ckd Severity
Investigators have also refined our understanding of the impact of AKI among CKD patients by examining the modification of AKIs effect by the severity of baseline CKD. Some earlier studies have emphasized that the superimposition of AKI on CKD greatly increases the risk of ESRD ,49 but the findings were based on diagnoses detected using administrative codes which are known to have important limitations.5457
Studies that used actual serum creatinine measurements to study this problem include that by Wu et al. who conducted a multiple-center study in Taiwan to directly compare acute on chronic kidney injury and de-novo AKI in intensive care unit patients who had undergone major surgery.58 The patients with acute on chronic kidney injury had a 20-fold higher risk of long-term dialysis , compared to those with AKI without pre-existing CKD.
Don’t Miss: Can I Take Flomax Twice A Day For Kidney Stones
Ckd As A Risk Factor For Aki
The association between severity of CKD and risk of AKI has not been quantified until relatively recently. In 2008, Hsu et al. compared 1,746 hospitalized adult members of an integrated health care delivery system who developed dialysis-requiring AKI with 600,820 hospitalized members who did not, and showed that the adjusted odds ratios were significantly and progressively elevated from 2.0 for those with baseline eGFR 4559 ml/min/1.73m2 up to 40.1 for those with baseline eGFR < 15 ml/min/1.73m2, when compared to referent patients with baseline eGFR 60 ml/min/1.73m2.5 This paper was also the first to report that proteinuria was a strong risk factor for AKI .5
The latter association that proteinuria is a risk factor for AKI–had not previously been appreciated, but has since been confirmed in a number of subsequent publications.17 These studies advanced the field by quantifying proteinuria closer in time to the event precipitating AKI , by more precisely quantifying proteinuria down into the microalbuminuria range19 and by examining other community-based populations.20 A number of meta-analyses have now been published characterizing how AKI risk is independently determined by severity of CKDdefined on two orthogonal dimensionsestimated GFR and albuminuria21 and describing how associations may vary in important subgroups.22,23